Disha Kansara Chawla of Mumbai doesn’t consult a doctor for relief from minor ailments. Chawla, who works in an executive recruitment firm, relies on her local chemist for medicines to tackle headaches, stomach cramps, back pain and even sore throat. “I have really crazy deadlines and by the time I come home it is late to see a doctor,” she says. “So I just call up my chemist and he sends me the medicine I need.” From painkillers to medicines for minor aches, Chawla, 31, finds relief over the counter.
Her mother, Rita Kansara, too, does not seek expert advice before popping painkillers. The 55-year-old homemaker says she doesn't have the time for rest in case of a headache or body ache and so she pops painkiller combiflam to keep up with the household work. Kamal Sonawane, 50, has chronic knee pain. So she relies on painkillers to stay on her feet. “When the pain becomes uncontrollable, I take four painkillers a day,” says Sonawane, who lives in Mumbai.
Most of us are guilty of popping over-the-counter drugs when we suffer from minor ailments. The common belief is, why would anyone go to a doctor when a Rs.5 tablet can take care of headache, backache, body ache, menstrual cramps and even migraine attacks? Most people rely on their chemist to suggest a drug during times of need. Analgesics or painkillers like aspirin, paracetamol, diclofenac, naproxen and ibuprofen are easily available and we pop them without batting an eyelid.
If these drugs are widely available and have been in use for so long, there could be nothing wrong in taking them, right? Wrong. Painkillers, like all other drugs, have side effects and popping them regularly and for a long time without consulting a doctor could lead to severe long-term damage. The most common side effects are heartburn, nausea and vomiting, but it could also lead to serious complications like liver and kidney failure or even stroke. The side effects usually depend on the type of painkiller.
“There are two major types of painkillers—opioid analgesics and NSAIDs (nonsteroidal anti-inflammatory drugs),” says Dr S.B. Patel, professor and head of pharmacology at Sir JJ Group of Hospitals in Mumbai. “Opioids act on the central nervous system and include drugs like morphine, pethidine and pentazocine. NSAIDS act peripherally and decrease the mediators of inflammation ie, substances that accumulate in the part of the body where we get an injury, and are responsible for producing pain and swelling."
The NSAIDs are further divided into selective and nonselective COX-2 inhibitors. Nonselective COX-2 inhibitors include drugs like aspirin, paracetamol, diclofenac, piroxicam and mefenamic acid though paracetamol is considered to be another category of drug because it reduces pain but not inflammation. Selective inhibitors include celecoxib, rofecoxib and valdecoxib.
Both types have side effects. “Opioid analgesics are associated with side effects on the central nervous system. They can produce dependence and addiction liability when taken for longer duration,” says Dr Shyamal Sinha, assistant professor of pharmacology at JJ Hospital. “They can also cause respiratory depression and can be potentially fatal if consumed in large quantities.” This is the reason why there is restriction on the sale of opioid analgesics; they are prescription drugs sold only in large hospitals. They are used only when other analgesics fail to work for very severe pain.
 Dr Bharat Shah
Dr Bharat Shah
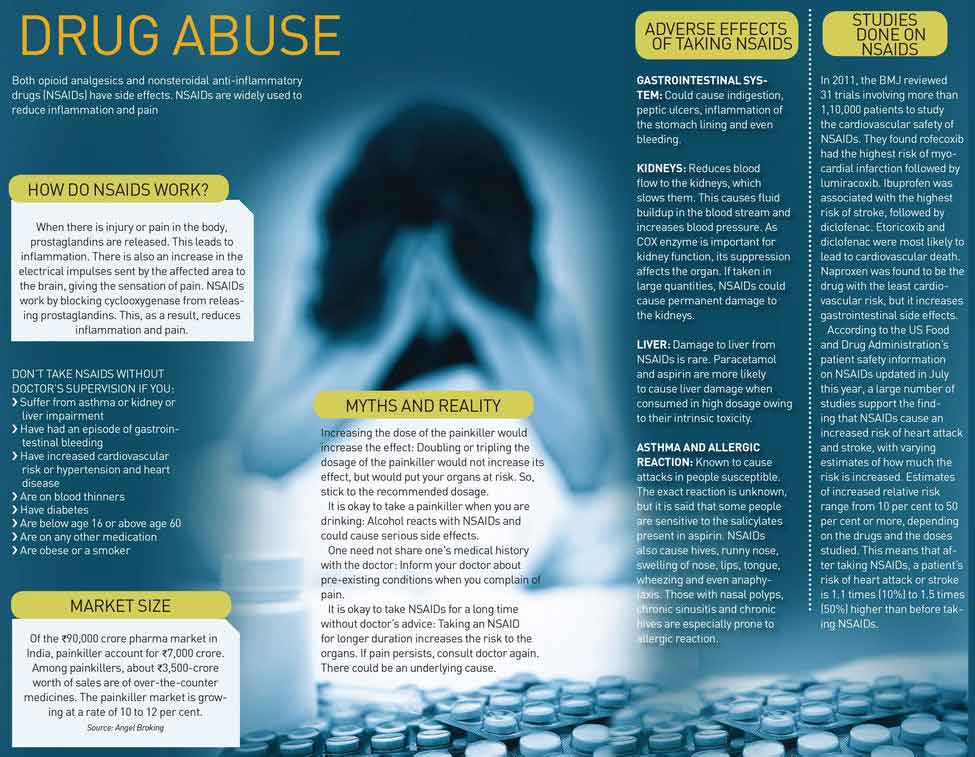
NSAIDs are widely used and effective in reducing inflammation and pain. The drugs work by interfering with the functioning of enzyme cyclooxygenase (COX). The enzyme controls the production of prostaglandins. Prostaglandin is a compound that causes inflammation or swelling and sensation of pain. However, prostaglandins also perform other important functions like protecting the stomach lining from gastric acids. Taking NSAIDs, therefore, has side effects like indigestion and stomach ulcers. Scientists then found another group of NSAIDs called COX-2 inhibitors, which do not affect the stomach lining but reduce inflammation and pain.
However, NSAIDs are under the scanner once again for their side effects. “NSAIDS are associated with gastrointestinal side effects, which include nausea, vomiting, gastritis, burning sensation in abdominal region and can produce ulcers in the gastrointestinal tract and cause gastrointestinal bleeds, which can present as blood in vomit or stool,” says Sinha. “When taken for a longer duration, they could also damage the kidney.”
Patients who consume OTC painkillers regularly without medical supervision are at risk. The painkiller market in India is worth Rs.7,000 crore, says Sarabjit Kour Nangra, senior vice president, Angel Broking. Of this, over-the-counter medicines account for sales worth about Rs.3,500-crore. “The painkiller market is growing at a rate of 10 to 12 per cent,” she says.
Most people assume that the chemist knows everything about the drugs just because he is selling them. “Just because the person is familiar with the drug does not mean that he has full knowledge about it,” says Dr Nilen Shah, orthopaedic surgeon at Wockhardt Hospital, Mumbai. “Yet, we see that though the chemists prescribe drugs, they are unwilling to take any responsibility if things go wrong.”
There is nothing like a safe painkiller, say experts, since each has a different function and if used correctly for the right duration, it could be extremely effective. Most doctors agree that paracetamol is safer of the lot with least side effects. However, taking more than the permissible dose—eight tablets a day—of paracetamol could be harmful for the liver.
In March, the Indian Medical Association asked the public to avoid self-medication with paracetamol and aspirin. “Aspirin cannot be given to children since it can cause Reye’s Syndrome or liver damage and it could also be especially damaging to the gastrointestinal system,” says Dr K.K. Aggarwal, honorary secretary general of IMA. “On the other hand, paracetamol in higher doses can cause liver injury and if taken with alcohol it can be dangerous.”
Since gastrointestinal problems are among the most common side effects of NSAIDs, a proton pump inhibitor, too, is usually prescribed to reduce the production of acid in the stomach. NSAIDs could also lead to abdominal bleeding which may require endoscopy, rescue therapy or even surgery. Dr Tariq Patel, gastroenterologist at Wockhardt Hospital, Mumbai, sees at least one patient a week who suffers from bleeding owing to painkiller consumption, that requires urgent intervention. In a patient who is already battling peptic ulcers caused by the H. pylori bacteria, the painkillers would aggravate the ulcers. Popping painkillers is especially dangerous for the elderly since they may have atherosclerotic arteries (plaque buildup in the arteries) which, coupled with bleeding, could cause serious complications.
A major cause for concern is that as painkillers provide instant but temporary relief, most people rely on them without actually going to the root of the problem. According to Dr P.N. Renjen, senior consultant neurologist at Indraprastha Apollo Hospitals in New Delhi, while people may pop a painkiller to stop a headache, taking painkillers for long could itself cause rebound headache. Also, many a times, high blood pressure or sinusitis, which cannot be resolved with a painkiller, may be the cause.
 Dr Vaishali Solao
Dr Vaishali Solao
“If the pain persists for more than five days even after taking the painkiller, it is advisable to see a doctor than just popping the pills,” says Dr Khusrav Bajan, intensivist at PD Hinduja Hospital, Mumbai. “Ideally, one must not consume more than 5 to 10 painkillers in a month,” he says. People with risk factors like diabetes, previous history of heart attack, stroke, kidney and liver disease or who smoke should take a painkiller only under the supervision of a doctor. Those suffering from chronic ailments like rheumatoid arthritis, osteoarthritis and fibromyalgia are prescribed painkillers. They should follow it up with the doctor and undergo regular tests to check their kidneys. “Many patients do not know that consuming a painkiller when they are dehydrated could severely affect their kidneys,” says Bajan.
While taking painkillers regularly could have serious side effects, in some cases even a tablet or two could make things to go wrong, as former chief secretary of Maharashtra Arun Bongirwar found out. A diabetic for the past 35 years, Bongirwar, 72, was asked by Dr Jatin Kothari, consultant nephrologist and transplant physician at PD Hinduja Hospital, to control his salt and water intake and not take painkillers. When he had thigh ache three years ago, the orthopaedic surgeon he consulted told him the pain was not associated with the bones but could be controlled with a painkiller, which he prescribed for three days. Bongirwar had taken just two tablets when he developed swelling in his feet. He rushed to Hinduja Hospital where doctors found that his creatinine levels had shot up to 4 from the normal level of 1.4, signalling deteriorating kidney function.
“I was admitted in the hospital for two days for the doctors to bring back the creatinine level to normal,” says Bongirwar, who is shocked by the damage that the painkiller did to his kidneys. He has not had the medicine since then. “I am lucky I didn’t need dialysis and my kidneys did not suffer long-term damage,” he says.
“It is the consumption of medication, be it painkillers or ayurvedic medicines that is responsible in almost 5 per cent of all kidney failure cases,” says Kothari. While Bongirwar was lucky that he didn't have any long-term damage, there are patients who suffer from permanent renal failure and are now dependent on dialysis. “No one thinks twice about popping a Rs.5 painkiller, but they should know that they will spend more money on treating the health problems caused by the habit,” says Kothari.
While the harmful effects of NSAIDs on gastrointestinal tract, kidney and liver are well known, warnings have been issued regarding the increased risk of heart attack and stroke after taking NSAIDs.
According to the FDA, the risk owing to the consumption of NSAIDs is 10 per cent to 50 per cent more than before taking an NSAID, depending on the drugs and the doses studied. The FDA routinely monitors and evaluates data regarding drug products, and new data from many observational epidemiological studies and a recent meta-analysis of randomised controlled trials provides stronger evidence of the increased risk of heart attack, stroke and congestive heart failure in non-aspirin NSAID users.
“These serious side effects can occur as early in the use of an NSAID as the first weeks, and the risk may increase the longer you are taking an NSAID,” says Eric J. Pahon, representative of the FDA, which in July issued an order to NSAID brands to add a warning on their labels. “The increased risk most often occurs at higher doses, so use the lowest effective dose for the shortest possible time.”
The additional risk posed by painkillers to heart patients has always been a cause for concern for cardiologists. “There is absolutely no awareness about the risks involved in popping a painkiller,” says Dr Vijay Surase, interventional cardiologist at Jupiter Hospital in Thane. “Painkillers mask the chest pain and the patient may be misguided and feel better while the painkiller actually causes damage to the heart muscle, which causes the heart vessel to rupture.” Surase had a 54-year-old patient who was diagnosed with multiple blockages in the heart and took painkillers every few hours against the doctor’s advice to deal with pain in his chest. He got himself discharged from the hospital, promising to return after three days. A week later, he was hospitalised in a critical condition. His heart vessel ruptured and he died within 24 hours.
“Patients with a history of heart attack and stroke are prescribed blood thinners, which react with NSAIDs and cause fatal bleeding. Hence we counsel all heart patients to not take a painkiller without consulting a doctor,” says Dr Upendra Kaul, executive director and dean, Fortis Escorts Heart Institute, New Delhi.
Not just over-the-counter usage, painkillers when given by medical practitioners without discretion could also be dangerous, Dr Vaishali Solao, senior consultant intensivist in the department of hepatology, liver intensive care and transplant of Hepatology Global Hospitals, Mumbai. “In many tier 1 and tier 2 cities, general practitioners still give loose tablets without prescriptions,” she says. “We have had patients coming to us with liver failure and on taking the history we realise they had taken some tablets given by the doctor and assume there was a painkiller in it since there is no way to ascertain for sure.”
 Dr Upendra Kaul
Dr Upendra Kaul
Anita Kumar (name changed) of Mumbai did not know she had been prescribed painkillers until her family physician asked her to do a kidney function test. A mother of two, Kumar was asked to take the painkillers by an orthopaedic after she complained of back pain and body pain post pregnancy. Diagnosing it as arthritis, the doctor put Kumar, 35, on painkillers which she continued to take for one-and-half years. “I didn’t get any relief but after taking the painkillers, I lost my appetite and energy,” says Kumar. She consulted another specialist, who said she did not have arthritis. Further tests revealed that her creatinine level was very high. The doctor told her that she had progressive kidney disease which may require a transplant later on. “There are many instances when the doctor prescribes a painkiller without knowing about the underlying kidney disease, which leads to serious health problem for the patient,” says Dr Bharat Shah, director of Institute of Renal Sciences at Global Hospitals. “So, doctors should order a kidney function test—a simple blood test—before prescribing painkillers.”
While it is impossible to curb the sale of painkillers over the counter, there could be ways to educate the public and create awareness. “Chemists can be instrumental in educating patients and warning patients who are diabetic, suffer from kidney failure or the elderly,” says Solao. “A regulation to curb the unrestricted use of painkillers would be welcome. The government could restrict the supply of painkillers.”
While talking about the risks involved, it is important to remember the crucial role of painkillers in mitigating pain, one of the most common debilitating symptoms that can affect productivity and quality of life. Also, in a country with poor doctor-to-patient ratio, it would be naive to expect a patient to consult a doctor for every ailment. Yet, doctors advice extra caution in view of the side effects. Take painkillers only when absolutely necessary, they say, for a short duration and consult a doctor if the pain doesn’t subside in a few days.