Interview/ Dr Sattva S. Neelapu, professor, department oflymphoma-myeloma, division of cancer medicine, The University of Texas MD Anderson Cancer Center
Dr Sattva S. Neelapu is a leading global expert in advanced cancer treatment methods like CAR T-cell therapy, which is transforming cancer care. He spoke to THE WEEK on the sidelines of Cura Immunis, a national conclave on CAR-T cell therapy held at the Medical Trust Hospital in Kochi. Excerpts:
Q/ Could you explain the science behind the CAR T-cell therapy?
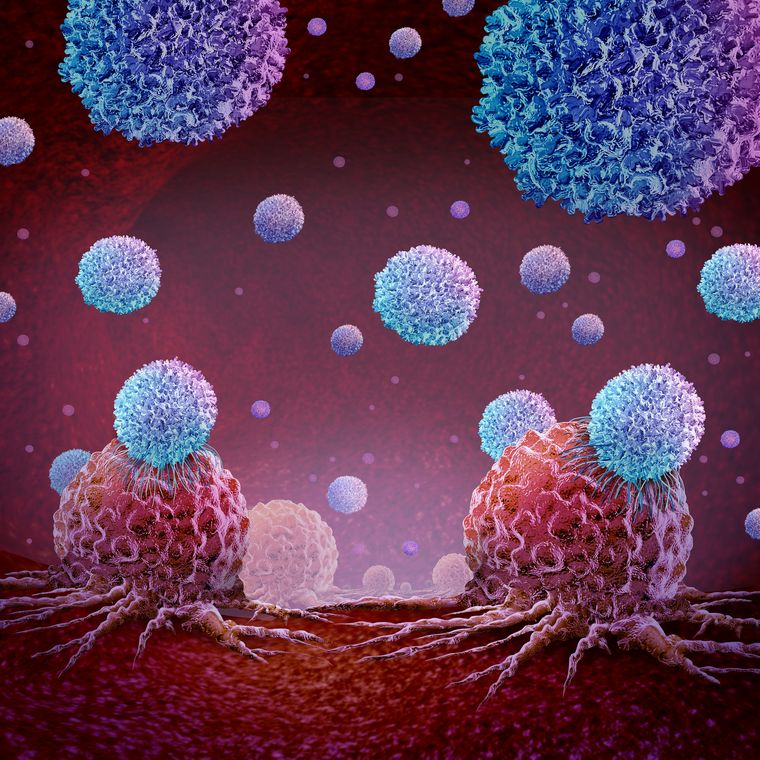
A/ CAR T-cell therapy is a form of genetically engineered T-cell therapy. The goal is to harness the power of the immune system to treat cancer.
We begin by harvesting T cells, which are a type of immune cell in the body. Then, using a virus as a vehicle, we introduce an artificial receptor into these T cells. This artificial receptor functions like a heat-seeking device—it is designed to recognise a specific molecule found on the surface of cancer cells.
Once the modified T cell encounters a cancer cell carrying that target molecule, the receptor activates the T cell. This triggers the T cell to attack and kill the tumour cell.
In that sense, it is often referred to as a “living drug”. After we infuse these modified cells back into the patient, they can multiply into billions and travel throughout the body to hunt down and destroy cancer cells.
Q/ What advantages does this therapy offer compared with traditional treatments like chemotherapy or radiation? With chemotherapy, for instance, it is more or less like 'carpet-bombing'. How is CAR T-cell therapy different?
A/ Right. So, this therapy was initially approved for use in patients who had already failed standard treatments, including chemotherapy and radiation—especially in cases like lymphomas and leukaemia. It is considered a completely different modality—this is immunotherapy.
One of the key advantages is that it does not cause the standard side effects typically associated with chemotherapy and radiation. And because it is a living therapy, these CAR T-cells can remain in the body for months or even years. In fact, there is data showing that these cells can persist for over 10 years.
Q/ So it is like a one-time treatment?
A/ Exactly. In many cases, it is a “one-and-done” treatment. And because these engineered T cells remain active in the body, they act like an internal surveillance system, continually monitoring for cancer recurrence. That is one reason why the remission rates are higher with this therapy, and in some cases, it even offers the potential for a cure—especially when all other treatments have failed.
Q/ You mentioned that CAR T-cell therapy does not cause the side effects associated with traditional treatments, but what are the side effects of this modality?
A/ There are some short-term side effects, typically seen within the first two weeks after the infusion. This is because of the activation of the immune system. The most common is a flu-like illness during the first week—patients may develop fever, body aches, chills and sometimes even low blood pressure or difficulty breathing. This cluster of symptoms is known as cytokine release syndrome (CRS). It occurs because the activated T cells produce cytokines. CRS can affect anywhere from 50 per cent to 90 per cent of patients. It is generally manageable. We usually treat it with standard medications like paracetamol to control fever and anti-inflammatory drugs, if needed.
The second common side effect is neurological toxicity. Some patients may experience temporary confusion or difficulty speaking. This usually happens during the second week and is typically short-lived—lasting two to four days—and completely reversible.
However, after about three months, some patients may have a slightly increased risk of infections, such as sinus infections or bronchitis. This is because the immune system takes some time to fully recover. To manage that, we often prescribe prophylactic antiviral and antibiotic medications, and in some cases, intravenous immunoglobulin infusions.
Q/ What kind of cancers are currently being treated with CAR T-cell therapy? Is it effective for all types of cancers?
A/ Currently, in India, CAR T-cell therapy is primarily approved for B cell lymphomas and B cell leukaemias—specifically, B-cell non-Hodgkin lymphoma and B-cell acute lymphoblastic leukaemia. These cancers can occur in both adults and children.
There are also ongoing clinical trials to treat another form of cancer called multiple myeloma, which affects the bone marrow. In the US and some other countries, CAR T-cell products have already been approved for multiple myeloma. While it is not yet approved in India, trials are underway, and we expect it could receive approval here within the next year.
Q/ Do you see CAR T-cell therapy becoming standard treatment for more common cancers in the future?
A/ Yes, there are active efforts to develop CAR T-cell therapy for other solid tumours such as breast, lung, and kidney cancers. Clinical trials are ongoing, and while the results so far have been more challenging compared with blood cancers, progress is definitely being made. So yes, it is possible that over the next decade, CAR T-cell therapy could become a standard option for a broader range of cancers.
Q/ What are the unique challenges and opportunities in implementing CAR T-cell therapy in a country like India? Is it capital-intensive?
A/ Absolutely. One of the biggest challenges is cost. Unlike traditional drugs, which are off-the-shelf products, CAR T-cell therapy is made individually for each patient using their own immune cells. That means every dose requires a separate manufacturing process, which includes genetic engineering—so, it is quite expensive.
The second challenge is time. Manufacturing the therapy for each patient typically takes three to four weeks. While many patients can be stabilised using other treatments during this period, not all can afford to wait.
The third challenge is infrastructure. CAR T-cell therapy cannot be administered just anywhere—it requires specialised transplant centres and highly trained physicians. The staff need to be equipped to anticipate and manage potential side effects like CRS and neurological toxicity. So at this stage, it is mostly available in advanced stem cell or bone marrow transplant centres.
Q/ So, in a way, this therapy reflects a broader shift in health care—moving away from the “one-size-fits-all” model to a more customised, patient-specific approach.
A/ Absolutely. CAR T-cell therapy is a form of personalised medicine. It is tailored to each individual because it is made from their own immune cells.
Personalised therapies can take many forms. Some target specific genetic mutations or molecular abnormalities in a patient's tumour. While CAR T cells do not target gene mutations directly, they do recognise and attack molecules specifically expressed on the patient’s cancer cells. So in that sense, it is still very much personalised.
The overall idea is that the more tailored the treatment is to an individual patient, the more effective and long-lasting the response is likely to be. That is the direction in which cancer treatment—and medicine in general—is heading.
Q/ How does CAR T-cell therapy improve the quality of life for patients compared with conventional treatments? Also, how soon can a person typically return to a normal, active life?
A/ That’s a great question—and definitely one of the major advantages of CAR T-cell therapy. As I mentioned earlier, it is typically a “one-and-done” treatment. The most intense side effects usually occur within the first two weeks, during which the patient is admitted to the hospital. Most patients recover to their baseline health within about a month after receiving the therapy.
Now, compare that to traditional treatments—chemotherapy regimens can last six months, and for some leukaemias, even one to two years. With CAR T-cell therapy, it is a single infusion, and the recovery timeline is much shorter.
In fact, studies in lymphoma patients have shown that recovery after CAR T-cell therapy is significantly faster compared with standard stem cell transplants, which involve high-dose chemotherapy and can take up to six additional months for patients to return to baseline. So yes, CAR T-cell therapy offers a much quicker and smoother path back to normal life and work.