John Smith is a healthy 56-year-old with no family history of cancer. Other than the occasional social drinking, he followed a healthy lifestyle, with regular exercise and a balanced diet. He never smoked.
Lately, he started getting up at night to urinate. He did not make much of it. But when he started noticing blood in the urine, he consulted a urologist. Following the prostate examination, which showed a hard nodule, the urologist ordered a blood prostate specific antigen test (PSA) test. The blood test revealed that his PSA level was very high. After an ultrasound, the urologist recommended a prostate biopsy.
A week later, Smith and his wife were sitting in the urologist’s office listening to alien terms like Gleason score, radical prostatectomy, radiation and hormonal blockade. The only word Smith heard and registered was prostate cancer.
Prostate cancer is a disease in which malignant cells develop in the prostate gland. The prostate is a small walnut-shaped gland that is a part of the male reproductive system. It produces some of the fluid that is a part of the semen that transports sperm during ejaculation. It is located just below the bladder and in front of the rectum. “Testosterone, the male hormone, acts like a food for prostate cancer,” explains Dr Jatin Bhatia, consultant-radiation oncology, Jupiter Hospital, Pune. “Testosterone gets converted into various chemical forms, and the form that acts as a feeder for prostate cancer increases. Meanwhile, the other forms decrease.”
Prostate cancer is the second most common cancer in men worldwide and the fourth most common cancer overall, after breast, lung and colorectal cancers. According to the World Health Organization, there were about 1.41 million newly diagnosed cases of prostate cancer in 2020.
Prostate cancer is less prevalent in Asia. It is more common in North America, northwestern Europe, Australia and on the Caribbean islands. While more intensive prostate cancer screening in many of the developed countries could probably be the reason, lifestyle factors such as diet and exercise could also play a role. For instance, while Asian Americans have a lower risk of prostate cancer compared to white Americans, their risk is greater compared to men of similar ethnic backgrounds living in Asia.
In India, one in every 10,000 men is diagnosed with prostate cancer, says Dr Ramakrishna Vangara, consultant-radiation oncologist, Manipal Hospitals, Vijayawada. According to data from national cancer registries, prostate is the second leading site of cancer among men in cities like Delhi, Kolkata and Pune and the third leading site of cancer in cities like Bengaluru and Mumbai. “With the increase in life expectancy, the incidence of prostate cancer has gone up phenomenally,” says Dr P.P. Singh, senior consultant and head of department of urology, PSRI Hospital, New Delhi.
Despite the increase in numbers, prostate cancer remains one of the least talked about cancers, at least in India. “Hence, there remains a great deal of misinformation about the disease and sometimes the symptoms are attributed to something else,” says Dr Ramesh Kinha, vice president and head of lab operations at Medall Healthcare in Chennai.
The exact aetiology of prostate cancer is unclear. Prostate cancer is caused when the DNA of a normal prostate cell starts to change. These gene changes can cause the cells to grow out of control and form tumours. Certain well-established risk factors for prostate cancer include advancing age, family history and certain genetic mutations.
“As we know, any cancer is from chronic inflammation. Inflammation could be caused by prostatitis. It could be even related to viral infections,” says Dr B.S. Ajaikumar, chairman and CEO, HCG Group of Hospitals, Bengaluru. “Over a period of time, these can cause prostate cancer. It can also be ethnic-based. It is also an ageing process.”
All men are at risk for prostate cancer, and the risk increases with age. About one in eight men will be diagnosed with prostate cancer during their lifetime in the US. Prostate cancer is rare in men younger than 40. About 60 per cent of cases are diagnosed in men 65 or older. The average age of men at the time of diagnosis is 66.
Prostate cancer can run in families. Having a first-degree relative (father, brother) with prostate cancer more than doubles a man’s risk of developing this cancer. The risk is also higher if several family members have had a diagnosis. That is one reason why Salil N.S., 52, a senior law officer at South Western Railway headquarters in Hubli, was not shocked when he was diagnosed. “This was not something alarming to me as I had other members in the family who had it, like my paternal uncle who has been living with prostate cancer for more than 15 years without any treatment,” he says. “The only difference was that he was diagnosed after the age of 65, whereas my diagnosis was before I turned 51.”
Several inherited gene mutations can also raise prostate cancer risk. Inherited mutations of the BRCA1 or BRCA2 genes, which are linked to an increased risk of breast and ovarian cancers, can also increase prostate cancer risk in men. Salil had a genetic profiling done, which indicated some mutations that could be the cause for his disease. Men with Lynch syndrome also have an increased risk for prostate cancer. Other contributing factors may include obesity, diet, hormones, smoking and alcohol consumption.
In general, prostate cancer grows very slowly and often does not cause any symptoms in its early stages. Symptoms of prostate cancer include problems with urination like difficulty starting urination, slow or interrupted urinary stream, frequent urination, especially at night, difficulty emptying the bladder, painful or burning urination, blood in the urine or semen and painful ejaculation. Symptoms of a more advanced prostate cancer that has spread outside of the prostate gland may include pain in the hips, back, pelvis, chest or other areas if the cancer has spread to bones, swelling or weakness or numbness in the legs or feet, weight loss, fatigue and loss of bladder or bowel control.
Prostate cancer often does not have any warning signs or symptoms. That is why screening and early detection are important. Cancer that is detected early, when it is still confined to the prostate gland, has the best chance for successful treatment.
The two most commonly used tests to screen for prostate cancer are PSA test and the digital rectal exam (DRE). Prostate-specific antigen test is a blood test that measures PSA levels in a person’s blood. The possibility for a cancer diagnosis increases as the PSA level goes up. Prostate cancer is commonly detected by elevated levels of prostate-specific antigen (PSA >4 ng/mL), says Dr Kirti Chadha, chief scientific officer and consultant onco-pathologist at Metropolis Healthcare, Mumbai. Men with a PSA level between 4 and 10 have about a 25 per cent chance of having prostate cancer. The chances of having prostate cancer are over 50 per cent if the PSA level is more than 10. But PSA levels alone cannot determine a cancer diagnosis. The PSA level could also be elevated due to other conditions that affect the prostate.
While screening can identify cancer early, the benefits may not always outweigh the risks. Both the PSA and DRE tests can yield false negative (a person may actually have cancer) and false positive test results (a person may not actually have cancer) and can often lead to unnecessary tests, like a biopsy of the prostate, as well as cause anxiety and confusion.
Screening can also lead to over-diagnosis and treatment. Since prostate cancer grows very slowly, some men with prostate cancer would never have had symptoms from their cancer nor would they die from it. Treatment of cancer that would never have caused a problem can lead to unnecessary complications from treatment like surgery and radiation, such as urinary incontinence, bowel problems and erectile dysfunction that can ruin a person’s quality of life, with no added benefit.
“The US National Cancer Institute does not have screening recommendations for prostate cancer. Prostate cancer screening should be done only after discussions with one’s doctors of the uncertainties, risks and potential benefits of screening,” says Dr James L. Gulley, chief of genitourinary malignancies branch and director of medical oncology service, National Cancer Institute, US.
If the PSA and DRE tests are abnormal, a prostate biopsy is often recommended. Prostate cancer is assigned a grade if the biopsy results show cancerous cells. The higher the grade the greater risk that the cancer is more likely to be aggressive and spread quickly.
A Gleason score is the most common scale used to determine the grade of prostate cancer cells. The score ranges from 2 to 10. A Gleason score of 6 or less indicates a low-grade prostate cancer; a score of 7 indicates an intermediate-grade cancer; and scores from 8 to 10 indicate high-grade cancer.
Once prostate cancer is diagnosed, other tests such as bone scan, ultrasound, CT scan, MRI or PET scans are done to determine if the cancer cells have spread to other parts of the body. This will help determine the stage of the cancer. Stage I means the cancer is confined to the prostate, while stage IV indicates the cancer may have spread to other areas of the body.
Treatment options depend on several factors, including the patient’s age, Gleason score, stage of the cancer, how aggressive the cancer is, whether it is confined to the prostate or has spread to other parts of the body, overall health of the person, as well as the potential benefits vs side effects of the treatment.
“We experience an unprecedented era of rapid new developments in the field of prostate cancer therapeutics, including radiopharmaceuticals/'theranostics' (using one radioactive drug to diagnose and another to deliver therapy), targeted therapies for selected patients (eg, PARP inhibitors) and novel immunotherapy strategies,” says Dr Petros Grivas, professor and clinical director, genitourinary cancers program, Fred Hutchinson Cancer Research Center, Seattle. “The advent of novel imaging, for eg Prostate Specific Membrane Antigen (PSMA) Imaging or fluciclovine/axumin PET, represents another great opportunity for more accurate prostate cancer staging. However, the clinical utility, impact and practical implications on decision making need to be better defined in clinical trials.”
Early stage, low-grade prostate cancer, especially in older men, may need minimal or even no treatment. Doctors may recommend active surveillance or watchful waiting. Active surveillance involves closely monitoring the prostate cancer by performing PSA tests and prostate biopsies regularly and opting for treatment if the cancer grows or causes symptoms. In watchful waiting, fewer tests are done. The patient is treated only if he has any symptoms. This is usually recommended for older patients with low-grade tumour.
But prostate cancer in younger patients and cancer that is aggressive need multidisciplinary treatments. A radical prostatectomy involves removing the prostate gland as well as some surrounding tissue and a few lymph nodes, an option for cancer that is confined to the prostate. Jitendra Yadav, 58, from Mumbai did a PSA test as part of his executive health check-up. Thanks to that, his cancer was detected early. “Also, the cancer was localised to prostate with no spread elsewhere in the body,” recalls Dr Shrikanth Atluri, uro-oncologist and robotic surgeon, Sir H.N. Reliance Foundation Hospital, Mumbai. “He was treated with robotic radical prostatectomy where the entire prostate was removed by surgery.” Yadav has been disease free for seven years.
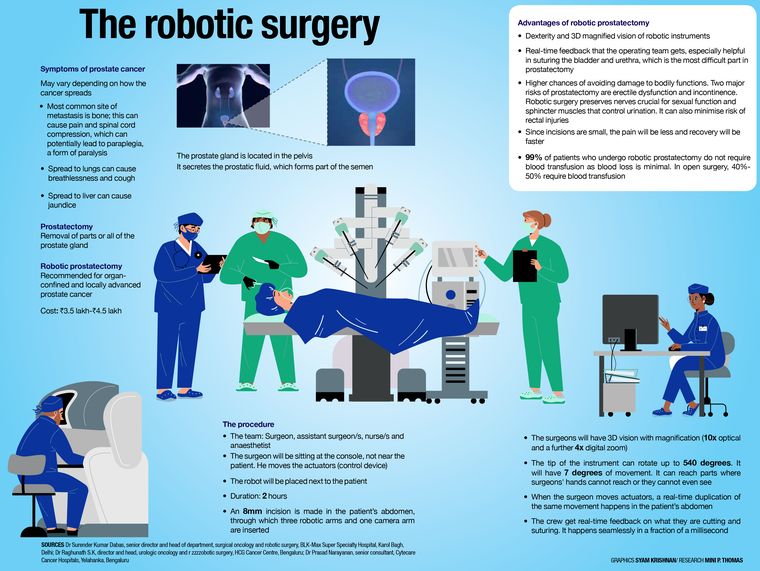
Novel surgical technologies such as laparoscopic and robotic surgeries to remove the prostate gland can potentially offer faster recovery and less complications. According to Dr Ashwin Tamhankar, consultant, uro-oncology and robotic surgery, Apollo Hospitals Navi Mumbai, surgeons prefer robotic surgery because it gives the advantage of better precision, control, 3D vision, negligible blood loss, quick recovery and early discharge.
Another treatment option is radiation therapy, which uses high energy rays to kill the cancer. There are various types of radiation therapy approaches like external beam radiation therapy, wherein a patient lies on a table, and a machine moves around the body, directing radiation at the cancer cells; brachytherapy (internal radiation therapy) involving small radioactive seeds or pellets that are surgically placed into or next to the tumour to destroy the cancer cells; and proton beam radiation therapy—a type of high-energy, external radiation therapy that uses streams of protons to kill tumour cells. There have been rapid advances in radiation therapy, like the CyberKnife device, which results in less damage to surrounding tissues when compared to conventional radiotherapy.
Apart from chemotherapy and immunotherapy, there are other therapies like cryotherapy, which uses extremely cold temperature to freeze and kill cancer cells, and hormone therapy that uses medications or surgery to reduce the levels of male hormones, called androgens, that fuel the growth of cancer cells in the body. There is also targeted drug therapy that uses drugs to target specific proteins that control the growth of the cancer cells. Bisphosphonate therapy has drugs, such as clodronate or zoledronate, that reduce bone disease when cancer has spread to the bones and reduce the risk of fractures. High-intensity focused ultrasound uses high-energy ultrasonic beams to kill cancer cells. And, photodynamic therapy uses a drug and a certain type of laser light to kill cancer cells.
Since Salil’s cancer had spread to the lymph nodes, he had a combination of therapies at HCG Bengaluru. His PSA levels were brought under control with hormone therapy. “Initially, surgery was being planned,” he says. “However, the decision was left to an interdisciplinary medical board. As the disease had responded well to hormonal treatment, the medical board advised to go for radiotherapy through CyberKnife.” His treatment lasted six weeks. “There is no significant weakness or other problems related to this radiation therapy,” says Salil. “It is a painless outpatient process. I was at the hospital alone during the treatment; no bystanders were needed.” The PSMA PET scan was repeated after the treatment. The results were heartening. However, Salil is still on hormonal therapy. “The treatment, particularly the hormonal therapy, has adverse effects on sexual life. Apart from that, life goes on as normal,” says Salil.
Novel treatments and technologies are changing the landscape of prostate cancer management. PARP inhibitors, such as Olaparib and rucaparib, are found to be highly effective in patients with genetic mutations such as BRCA1 and 2.
“PSMA PET scans are one of the most exciting recent developments in prostate cancer,” says Dr Rahul Tendulkar, clinical director and residency program director for the department of radiation oncology, Cleveland Clinic, US. “By detecting early recurrences while they are small in size and number, we can offer patients treatment with stereotactic body radiation therapy and hopefully eradicate their visible disease.”
Ramlal Sahu, 85, from Nagpur was suffering from frequent urination, difficulty in passing urine, back pain and pain in his left leg because of which he was unable to walk. He was admitted in a critical condition to HCG NCHRI Cancer Centre, Nagpur, and was diagnosed with prostate cancer. Sahu had multiple comorbidities such as diabetes and hypertension and he also suffered from cardiac-related issues, which prevented him from being a candidate for chemotherapy.
“We started him on targeted therapy and tested for genetic mutations and he tested positive,” says Dr Nikhil Pande, medical oncologist, HCG NCHRI Cancer Centre, Nagpur. “He is now on second-line treatment with Olaparib, a form of targeted therapy and is doing well.”
Chadha is thankful for scientific advances. “The gland’s location on the neck of the urethra by the bladder means that whole-gland treatments like radical prostatectomy or radiation therapy often leave men with incontinence and erectile dysfunction,” she says. “However, developments in MRI are enabling more targeted treatments to the prostate without damaging surrounding structures.”
Researchers are now testing the use of artificial intelligence to recognise suspicious areas in a prostate MRI that should be biopsied, says Chadha. “AI tools also help pathologists who aren’t prostate cancer experts to accurately assess prostate cancer grade,” she says.
Can prostate cancer be prevented? There is no absolute way to prevent prostate cancer. Risk factors such as age, genetics and family history cannot be modified. While several drugs and supplements are being studied, there isn’t enough evidence to make conclusive recommendations on prostate cancer prevention.
Maintaining a healthy weight, staying physically active, eating a balanced diet and avoiding smoking are all factors that could improve your overall health and lower your risk of prostate cancer.
Some studies have suggested that high consumption of dairy products may increase the risk of prostate cancer. Limiting dairy products and calcium intake could be beneficial.
A couple of studies have suggested that men with a higher frequency of ejaculation may have a lower risk.
Since prostate cancer tends to grow slowly, most men diagnosed with prostate cancer will live a long, normal life and do not die from it. The 10-year survival rate is about 98 per cent. Many of the elderly men detected with prostate cancer die with prostate cancer rather than because of it, says Bhatia.
There are hundreds of clinical trials in different phases related to prostate cancer treatment that are in progress around the world. These trials will help the medical community better understand how to diagnose, treat and prevent prostate cancer and improve patient outcomes.
“While significant strides have been made in treating localised and advanced prostate cancer, understanding the disparities in prostate cancer outcomes by age, stage, race and ethnicity is crucial to decreasing global incidence of prostate cancer, especially in developing countries” says Dr Shilpa Gupta, director of genitourinary oncology program, Cleveland Clinic.
Some names have been changed.