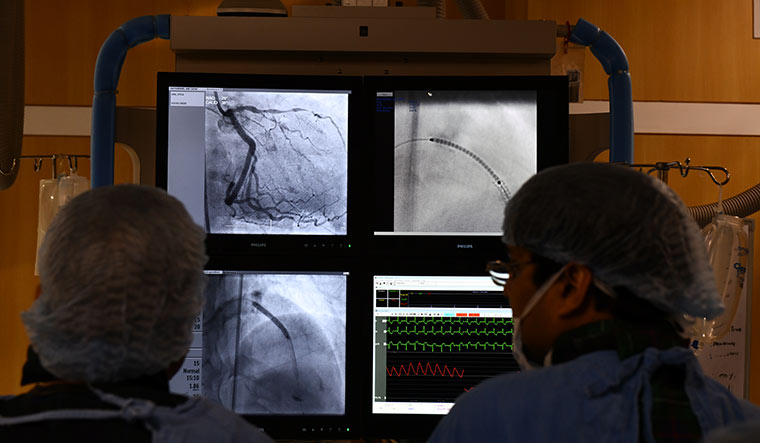
Inside the chambers of Dr T.S. Kler, chairman of PSRI Heart Institute, Delhi, it is a typical Wednesday. At about 10.30am, patients begin to stream in. The complaints are varied, ranging from shortness of breath, palpitations, a fit of epilepsy (a young man's parent worries if it could be a heart-related ailment), to a man who has brought in an angiogram of his father in his mid-50s. A quick flip through the images and the cardiologist delivers his assessment—the condition of the patient’s heart is beyond the angioplasty stage; he will need a bypass surgery, immediately.
Minutes after finalising a date for the surgery, Kler is weighing on the relative merits of routine invasive procedures for this interview—the efficacy of percutaneous coronary intervention (PCI), also known as coronary angioplasty, and coronary artery bypass surgery versus medicines and lifestyle changes among patients with stable heart disease.
The genesis of the discussion stems from the results of the largest clinical trial of its kind that had 5,179 patients from 320 sites from across the world—India was a top site for the study—and sought to evaluate the efficacy of routine invasive procedures over optimal medical therapy for patients of heart disease.
The International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA), as the trial is known as, was twice as large as any other similar trial done before. The crucial findings, now the subject of much debate and discussion, were presented at the annual conference of the American Heart Association, and are likely to be published over the next few months. The study failed to show that routine invasive therapy was associated with a reduction in major adverse ischaemic events when compared with optimal medical therapy among stable patients with moderate ischaemia (insufficient blood flow to the heart muscle).
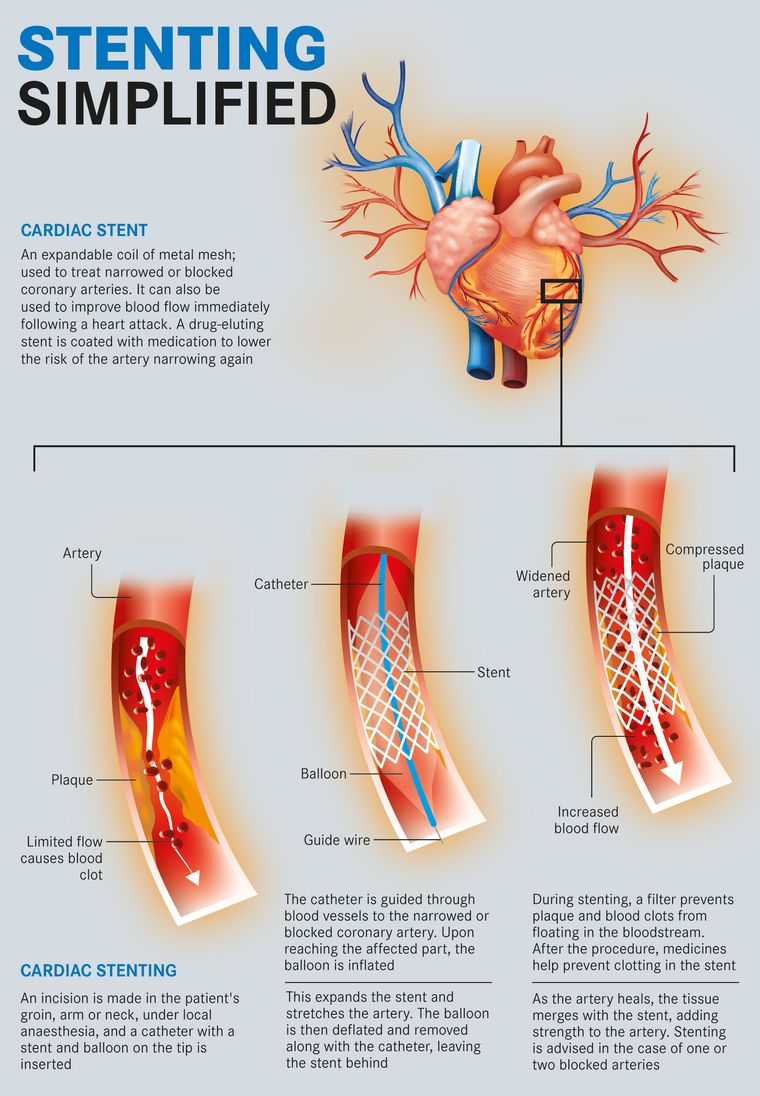
The randomised trial, funded by the National Heart, Lung and Blood Institute in the US, recruited 5,000-odd patients with stable heart disease, and divided them into two groups. The invasive strategy group underwent a surgery (stenting or bypass, as the case may be) after the stress test, and received drugs (statins inlcuded) and followed lifestyle changes to treat their blockages. The other group, however, received drugs and followed lifestyle changes only.
Both the groups were closely monitored for 3.3 years on average and 5 years maximum. The outcomes at the end roughly remained the same—events such as cardiovascular death, myocardial infarction (heart attack), resuscitated cardiac arrest, or hospitalisation for unstable angina or heart failure at 3.3 years occurred in 13.3 per cent of the routine invasive group, compared with 15.5 per cent of the medical therapy group. Invasive therapy, it was found, was associated with harm of about 2 per cent within the first six months. However, a benefit was observed within four years.
Put simply, the outcomes remained same regardless of whether patients had stenting or bypass surgery, bringing to fore an important question—do stents or bypass surgery work for a certain section of patients of heart disease?
Cardiologists in India caution against a simplistic interpretation of the finding and dismissing one therapy in favour of the other. The clinical decision on whether or not to go for a stent or bypass surgery would depend on several factors, they insist. At the outset, they point to the exclusions in the study. “While the trial does show that there is no need to do angioplasty on every patient who comes to a doctor with angina (chest pain), the trial subjects do not constitute the entire spectrum of patients with heart disease. Those with acute coronary heart disease were excluded from the study,”says Kler. Patients suffering from left main stenosis (narrowing of a valve), those who had suffered a heart attack recently, had severe angina and had undergone a stenting or a bypass in the last one year or patients of heart failure were not included in the study. In a country such as India, that would constitute a majority of heart patients, at least in a hospital in a metro such as Delhi.
India, says Kler, has an incidence of heart disease that is 2.5 times higher than in the west, and heart disease strikes patients here 10 years earlier than their counterparts in the west. In urban areas, heart disease incidence is found in 8-10 per cent of the population; in rural areas, it is 5-6 per cent of the population. Around 54 million people in India suffer from heart disease, a leading cause of death in the country. Over 80 per cent of these are patients with ischaemic heart disease and stroke.
Despite the numbers though, awareness and access remain an issue. At a public hospital such as AIIMS, Dr Ambuj Roy puts the ratio at 60:40 for those suffering acute coronary artery disease and those that have stable heart disease (where symptoms come only when you exercise or feel stressed). A majority of patients also come to the cardiologist late. “Several times, discomfort due to heart disease is dismissed as a gastric episode,” says Roy, professor of cardiology, AIIMS. “Patients with a heart attack often don’t get lifesaving surgery within the golden hour, causing permanent damage to the heart muscle.”
For patients whose disease is stable, the question of stenting or not has been controversial for a few years. In 2007, the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial, showed a similar outcome—as an initial management strategy in patients with stable coronary artery disease, PCI did not reduce the risk of death, myocardial infarction or other major cardiovascular events when added to optimal medical therapy. Later trials, including the ORBITA trial last year also showed similar results—in patients with medically treated angina and severe coronary stenosis, PCI did not increase exercise time any more than the effect of a placebo procedure did.
“The criticism against the earlier studies such as COURAGE was that they used the older generation of stents. However, this has been overcome with the ISCHEMIA trial where they used the latest generation of stents,”says Roy.
Most cardiologists agree that when it comes to patients with stable disease, there is no need to panic and opt for stenting or surgery immediately. “It also emphasises the need for aggressive medication (with four drugs including statins), and patient compliance to the drug regimen,”says Dr Ashok Seth, chairman and interventional cardiologist, Fortis Escorts hospital, Delhi. “During the trial, the patients on conservative therapy were followed up regularly and they stuck to the drug regimen and lifestyle changes that were suggested.”
The panic aside, Seth says the study also shows that stenting did improve quality of life for those with symptoms, and 25 per cent patients from the conservative group had to undergo routine invasive procedure at the end of four years. “The key takeaway from the study then is that stenting works if the patient reporting symptoms such as angina is young and leads an active lifestyle, if they have symptoms and live in a remote area from where they can’t access immediate medical care in case their symptoms worsen despite drugs, and if the procedure can be performed safely without risk of a heart attack during the procedure [because of multiple, diffuse blockages],”he says.
“It isn’t as if we weren’t following such a protocol before,”says Dr P.P. Mohanan, president-elect, Cardiology Society of India. “However, now with data, it will help both doctors and patients have an informed discussion about the future course of action in such cases,”he says.
Invasive procedures such as stenting have their benefits, but many cardiologists concede that the trend of unnecessary procedures does exist in India. “About 25-30 per cent invasive procedures in this field are unnecessary, and done for increasing revenues,”says Kler. “The only way to deal with such unethical practices is to have medical audits. The justification for doing a procedure might still be subjective in some cases, but for a majority of the cases, it will be easy to regulate.”
An industry official, however, bemoans the lack of guidelines in India for performing such procedures. “In the absence of such regulations, it is hard to dispute the placement of a stent or the justification of a bypass procedure,”he says. “The other side of the debate is that in India those who need a procedure such as stenting don’t get it. WHO figures suggest that of the 30 lakh people who have a heart attack, only 5 lakh reach a cath lab, and only 10 lakh get some form of medical treatment in the form of drugs to dissolve clots. Only 1,400 cath labs exist in the country.... Here, too, there are regional inequalities—a state like Bihar has only 15 cath labs, while an area like suburban Mumbai itself will have that many cath labs.”Also, there is the issue of affordability. “A developed state such as Gujarat has only two government hospitals where such a procedure can be performed,”he says. “And private hospitals will keep doing these procedures for profit.”
Every month, around 55,000-60,000 patients undergo angioplasties in hospitals around the country, industry estimates suggest. During these angioplasties, the number of stents used could vary from 65,000-75,000 (since more than one stent could be required for the procedure for patients with multiple blockages). The average ratio, industry sources suggest, works out to be 1.3 stents per procedure, and the coronary stent market stands at Rs1,500 crore.
India is the third largest market in terms of volume of stents after the US and China, but because of lower prices of stents (compared to the US and Europe) the total worth is less. When it comes to the number of stenting procedures done in a year, India is not far behind the US, where the number of angioplasties stand at about 10 lakh per year.
This year, Asia's largest stent manufacturing unit is set to come up at Hyderabad, which will cater to both the growing stent market in India and neighbouring countries. The unit is being set up by the Surat-based manufacturer Sahajanand Medical Technologies.
However, disparities in terms of reach and access to angioplasties continue to plague Indian patients. India has about 3,000 interventional cardiologists. The number of centres doing PCI in the US is around 1,758 for a population of 35 crore. Given India's 130 crore population, we need at least 6,000 labs as opposed to the 1,400 labs, says an industry official.
As of now, the stent market in India has both Indian and multinational players. Post price capping for coronary stents (bare metal and drug-eluting stent) in 2017, however, the MNCs have been finding it hard to expand their market, say industry sources. “Indian companies are supplying directly to the hospitals but the MNCs do it through distributors which makes their prices higher,”he says. “The trade margins for coronary stents were fixed precisely because the margins were found to be over 200 per cent in certain cases by the National Pharmaceutical and Pricing Authority. Thus, post price control, this business model has meant that the foreign players have not been able to grow or expand their market, especially outside the metros. They do supply directly to other hospitals in other countries. So why not here?”
Post the capping of prices, however, there were reports of hospitals making up for the loss in profits by revising the prices of other components in the angioplasty package. Patient advocates, however, argue that the lower price did increase the affordability of the procedure.
With the advent of Ayushman Bharat, where the government reimburses 070,000 for the angioplasty package (including one DES), the market is only set to grow, say sources. In the private sector, though, costs of the same procedure, however, could go upto Rs2 lakh.
But, how do patients decide between an invasive therapy and one that involves only medication and lifestyle changes? Dalchand Mohanpuri and his family had to make that choice last year. The 67-year-old retired income tax officer had started gasping for breath while climbing stairs to his third floor house in Delhi's Karol Bagh. A doctor at the nearby Central Government Health Scheme (CGHS) dispensary recommended he undergo certain tests to check his cardiac situation. The family, however, decided to go to a cardiologist at a prominent private hospital. “Initially, the cardiologist recommended that my father undergo an angioplasty procedure,” recalls Lokesh, Dalchand's son. Dalchand had suffered a heart attack about four years ago while undergoing treatment for dengue at a nursing home. The doctors at the nursing home didn't recommend any particular treatment. After an angiogram at the private hospital, doctors revised their opinion—the blockage in the arteries was too calcified, and Dalchand could neither undergo an angioplasty, nor was he a fit candidate for a bypass surgery. “He was then recommended a pacemaker. Alternatively, doctors said that we could opt for medicines only,”says Lokesh. The family opted for medication, and close monitoring of the situation. “Since then, my father is on medication for his diabetes, blood pressure, cholesterol and heart disease. He walks regularly, avoids oily food and tries to keep himself fit,” says Lokesh. “One year later, his condition has actually improved. From the earlier condition where doctors said only 35 per cent of his heart was good, they are now saying that it is about 45-50 per cent. In fact, now he might not need a pacemaker either.”
Lokesh says it is a tough call to make for any family. “My father is a CGHS beneficiary, and so any procedure is not easily approved and has to be justified. Had it not been the case I am sure that the doctors would have opted for an angioplasty and/or a pacemaker without enough justification,”says Lokesh, an engineer. “For lay persons, getting medical treatment or going for a procedure is an emotional decision, not a rational one. Accessing treatment at a government hospital is difficult because of long queues, and private hospitals are only going for profit. In that situation, for a patient to make a rational decision is just impossible.”
Dr Thomas Davis, however, did not face that dilemma. It was a typical day at the emergency room at Delhi’s Max hospital in 2003. Davis, then 38, was on duty, handling the rush of emergency patients. Little did he know that in the next few hours, he would become a patient. Davis had a heart attack that day, and then another one in 2013. “Both times my condition was acute, and there was absolutely no confusion in the line of treatment that was to be taken,”says Davis, who underwent angioplasty twice.
Patient advocates, however, stress on the need for counselling patients properly. “We are aware that many a time patients are recommended angioplasty even though the patient may have been a good candidate for recommending medication and lifestyle changes. This is often a result of doctors' perceptions about the patient’s ability to follow instructions or is simply justified as a pragmatic approach (for example, when patient has travelled from far for the consultation it could be justified as reducing inconvenience),”says Malini Aisola, All India Drug Action Network. “Without appropriate counselling, patients are not given a chance to participate in treatment decisions and are deprived of options in lieu of an invasive procedure.”
While he lay on the doctor’s table waiting for the procedure the second time, Davis says he made one decision that changed his life. “I was a heavy smoker. I had quit after the first heart attack, but somehow started smoking again three years later. But before the second procedure, I decided to quit forever, and since that day in 2013, I haven’t smoked even once,”he says.
The 55-year-old also made alterations in his diet—he gave up red meat, alcohol and increased the portion of vegetables, fruits and proteins in his meals. Other than that, Davis says he has been on statins, blood thinners and beta blockers. “I have been really compliant with my medicines, and never missed a single dose in all these years,”he says. What Davis does regret though is that given his hectic schedule inside the emergency room, he doesn’t get much time for exercise. “Whatever exercise I get is from the running around that we do during duty hours,”says Davis, who now works with a different hospital chain.
But Davis sees a lot of patients ending up with heart trouble in the emergency room, especially those in their 30s. “I tell them three things, give up smoking, reduce stress and make lifestyle changes,”he says.
That is some sound advice, especially the one about smoking. It is one of the top risk factors for heart disease, say doctors.
Though the ISCHEMIA trial focused on the outcomes and efficacy of coronary stents and bypass procedures, patients in both arms of the study—invasive or non-invasive—received optimal medical therapy that included aggressive medication and lifestyle changes. The drug therapy included anti-platelets, statins, antihypertensive and other lipid lowering and anti-ischaemic medical therapies. Drug therapy, say doctors, has to be aggressive, and patients need to comply with the regimen, too. Regardless of whether the patient has undergone a procedure, taking medicines and following a healthy lifestyle is key, they say. Quitting smoking is one of the major alterations advised. “I always ask my patients to pay attention to the six Ss—stress, sleep, smoking, sedentary lifestyle, sugar and salt. Less salt and sugar and regular exercise (45-50 minutes) everyday can help manage the disease to a great extent. In India now, pollution, akin to smoking, has also emerged as a big risk factor for heart disease,”says Dr Viveka Kumar, principal director of cardiac sciences and chief of Cath Labs Pan Max Healthcare.
Most individuals with stable ischaemic heart disease can be managed effectively with good and evidence-based medical treatment, says Dr Upendra Kaul, chairman, Batra Heart Centre. “This means keeping BP <130/80, blood sugar under control in diabetics, aggressive lowering of cholesterol levels by taking high dose of statins and taking anti-platelet drugs for the long term,”he says. Angioplasty and stent implantation are reserved for patients with increasing symptoms or for persons who want to be physically active for improving quality of life, says Kaul. “The goals of treatment [in chronic stable heart disease] are to prevent a heart attack, sudden death and heart failure. These goals are not achieved better by angioplasty or bypass surgery in stable patients,”he says. “Some patients with angina also get it because of inadequate dilatation of micro vessels well away from the site of major blocks. Such subtle changes can be diagnosed by PET scans and are of academic interest only.”
According to Kaul, it is a scientifically proven fact that acute heart attacks do not occur in chronically blocked arteries. The most common cause is rupture of a cholesterol rich plaque that is thin walled; once it ruptures, a clot forms at that site. “This leads to a sudden blockage of the artery leading to a cessation of blood supply to a portion of the heart,”he says. “The size of the heart attack depends upon the size of the artery and its location. This is sometimes also seen in patients who recently had angiography done and were labelled as nearly normal. The control of risk factors is crucial in such patients along with a good lifestyle.”
The management has to be lifelong and sustained. All high-risk patients like diabetics, patients of high BP or raised cholesterol levels need this management. Says Kaul: “Optimal medical treatment for stable heart disease is definitely more important than angioplasty or bypass surgery.”