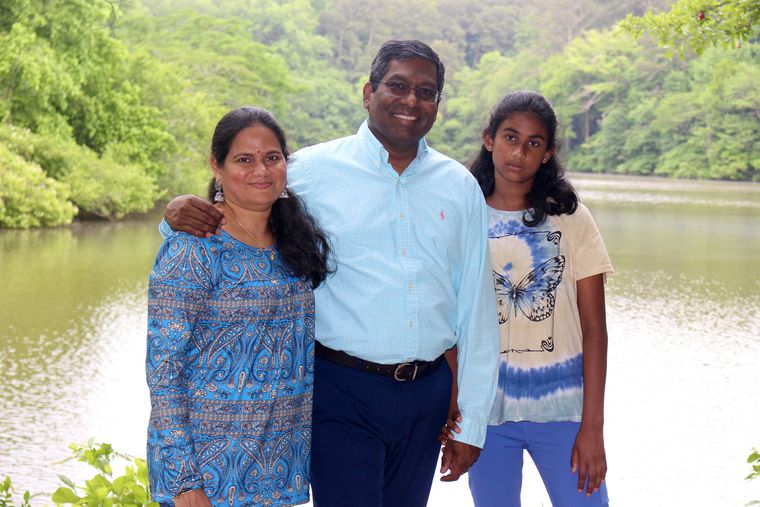
As the aroma of freshly brewed coffee seeps into his cubicle, Prof Rama Rao Amara remembers that he has not had his lunch. Amara, 52, from Kavali in Nellore district of Andhra Pradesh, says that he has become forgetful of late. “At times, I leave my daughter's school bag behind while dropping her off at school,” he says with a smile as he makes me a cup of coffee. The self-confessed movie buff and cricket fan is now completely immersed in his work—an HIV vaccine project.
A Charles Howard Candler professor of microbiology and immunology at the Yerkes National Primate Research Center, Emory University in Atlanta, Amara has made much headway with his research. The laboratory he works with is developing prophylactic (preventive) vaccines to block HIV infection, and immunotherapy to treat people infected with HIV. The improved versions of HIV vaccine candidates developed by Amara can prevent infections with 70 per cent success in rhesus monkeys. In his study, the animals were exposed to the virus six times. The monkeys that were not vaccinated were all infected after the third exposure and 70 per cent of vaccinated animals were unaffected after the sixth exposure.
These improved vaccines are known as adjuvanted DNA/MVA vaccines. Adjuvant is an agent used to create a stronger immune response. MVA—modified vaccinia virus ankara—is a modified smallpox viral vector that holds many advantages as a vehicle for delivery of HIV antigens. Plans were underway to start the phase-1 human trials when Covid-19 struck and pushed things behind schedule. (Amara's laboratory quickly used the same platform to develop a Covid-19 vaccine that showed great promise in primate studies.)
The human trials of earlier versions of DNA/MVA vaccines that Amara co-developed with his postdoctoral mentor Prof Harriet Robinson offer much hope for people with HIV. A study conducted by Geovax, a biotechnology company working with HIV Vaccine Trials Network—a US government funded body that conducts HIV vaccine trials—found that DNA/MVA vaccines are safe and that they generate the desired immune responses in human beings. Emory University has licensed the technology to Geovax and the company is now working to begin efficacy trials.
Amara's laboratory, in an alternate approach to treat HIV-infected individuals, alsoshowed that giving vaccine to animals after they are infected and treated with anti-HIV drugs can control the virus even after discontinuation of the drugs.
So does this mean HIV infection can be cured? “A complete cure means there is no virus in the person's body,” says Amara. “I don't think that is feasible right now. What we offer is a functional cure, which enables a person with HIV to lead a normal life. There could be a low level of virus in their body. But they do not transmit the virus, and they do not have to be on drugs. That is possible. We are trying to reprogramme their immune cells in such a way that they can actually fight the infection.”
According to the India HIV Estimation 2015 report released by the National AIDS Control Organization, India has about 21.17 lakh people living with HIV. Two-fifths (40.5 per cent) of them are women and children below 15 constitute 6.54 per cent.
“A vaccine for HIV is the need of the hour,” says Dr Diwakar Tejaswi, an HIV specialist and member of the governing body of the Bihar State AIDS Control Society. “There have been a few HIV vaccine trials in the past, including the much-hyped RV 144, but no major breakthrough yet. However, we are optimistic.”
Like Amara, the subjects used in his animal trials also have an Indian connection. “[The rhesus monkeys] were brought from India long ago,” says Amara. “We breed them at our Primate Research Center field station in Lawrenceville, which is about 25 miles from the main centre of Yerkes. They live in colonies. We take good care of them.”
The monkeys are used in such studies because HIV does not infect mice or other small animals. “So, for studies on HIV, primates, especially the Indian rhesus monkeys, are the ideal animal model,” says Amara. The pathogenesis differs depending on the primate used. “For instance, sooty mangabey monkeys also get infected with HIV, but they don't develop AIDS,” he says. In Indian rhesus monkeys, SIV—Simian Immunodeficiency Virus—duplicates the symptoms and the disease as in humans. Amara adds that disease progression in Indian rhesus monkeys is also faster because the virus grows to 10 times the levels that is normally seen in humans.
Vaccines are considered the best tool for controlling HIV. “The development of a vaccine is the only way you can prevent HIV transmission efficiently,” says Amara. Though people can do “pre-exposure prophylaxis”, such as taking anti-HIV drugs before having sex, they have to remember to do it, he says. “When you have a vaccine, you ideally do not have to take any precautions,” he adds. “That is the kind of vaccine we are talking about. And then it is cheap. So, typically you just have to take three or four shots.”
The DNA/MVA vaccines being developed by Amara are based on the concept of immunological memory. “[Some] cells can remember what they saw before,” says Amara. “Our vaccine centre director and colleague, Prof Rafi Ahmed, is a world leader in this area and has done great work on how these memory cells are formed. They can respond rapidly and clear the infection fast.”
The vaccines contain “pieces of HIV”, which trick the body into generating an immune response to the HIV infection. When you get infected, the white blood cells in your body start to divide and replicate themselves. So there are more soldiers to fight. Under normal conditions, the number of white blood cells in your body that can fight against one particular infection could be about one out of 10,000 or 1,00,000. “If you do not have enough soldiers to counter the attack, then the virus wins,” says Amara. “But if you have more soldiers, the host wins. You just prepare yourself for a future attack, have more numbers ready for you who can act very fast, and when the virus comes, you kill it.”
Phase-2A trials of the vaccines are complete, but Amara knows that phase-2B studies that involve efficacy trials in humans could be more difficult. Researchers typically vaccinate human subjects and then expose them to the virus. But since there is no cure for the disease, such trials are all the more challenging when it comes to the HIV vaccine. As a solution to this research obstacle, clinical trials are done in areas where the transmission rate is high. Researchers randomly vaccinate thousands of people. Another group in the same locality will receive placebos.
“And then you watch over three years what happens to transmissions,” says Amara. “In the vaccine group, we should see a dramatic reduction in transmission. These experiments need a large number of people and are expensive.” Amara adds that for phase-3 studies he is planning to go outside the US to pockets where the transmission rate is as high as 25 per cent. Another hurdle that HIV researchers face is that the vaccine has to be widely effective as the virus is “genetically variable and different” all over the world. “They have different properties. So we need to overcome that diversity and deal with those different variants,” says Cynthia Ann Derdeyn, professor, laboratory medicine and pathology, University of Washington.
The vaccine can be a boon for HIV's unsuspecting victims. In India, there have been numerous instances where blood transfusions caused HIV infection. There is a risk of transmitting the virus through blood transfusion if the donor is in the “window period” when screening tests on donated blood may not detect the presence of HIV.
Maya (name changed), from Alappuzha, Kerala, contracted HIV allegedly after getting a transfusion at the Regional Cancer Centre in Thiruvananthapuram. The nine-year-old who was being treated for leukaemia passed away due to pneumonia. RCC had apparently complied with all the guidelines for safe blood transfusion stipulated by the National AIDS Control Society and the World Health Organization.
A report of the Kerala State AIDS Control Society revealed that the girl had received blood from 48 people, of whom one was HIV positive. He was in the window period at the time of blood transfusion. Maya's father Shiji C. says the hospital officials concealed that his daughter contracted HIV from a blood donor. “There is enough evidence to believe that there was a lack of transparency on the part of the hospital officials,” says the daily-wager. “They would have thought my daughter might not live long and that we would give up. And one cannot help but wonder why they took so long to confirm her HIV status.”
Gyan Ranjan from Patna contracted HIV through a blood transfusion, at a clinic, following an accident. He went into depression and locked himself in a room for two weeks after he tested positive for HIV. Ranjan got Covid-19 and died in 2021 in his mid forties, but he was excited at the very prospect of an HIV vaccine and believed that it would save the lives of many people who shared his fate.
Dr V.D. Ramanathan, who was a director-grade scientist at the Indian Council of Medical Research, says that Amara's “pioneering work” is of great relevance to India in the context of the focus on HIV prevention. Ramanathan, who was principal investigator for two phase-1 HIV vaccine trials in India and was also involved in evaluating newer anti-TB vaccines in animal models, adds that Amara's work on immunotherapy for those infected by HIV will also be of immense value as it will arrest the disease.
Dr Sunil K. Arora, a professor of immunology and head of the department of translational and regenerative medicine at the Postgraduate Institute of Medical Education and Research, Chandigarh, says the vaccine approach looks promising. “But, we may have to wait for the human trials to show their efficacy,” he adds.
For Amara, the vaccine is a tribute to his late father, who wanted him to take up medicine. “He would always say it is a noble profession that can save lives,” recalls Amara, who lost his dad when he was 17. Amara narrowly missed out on admission for medicine and ended up opting for biotechnology. He loved biology and was fascinated by how our immune system fights infections. For his PhD, Amara worked on tuberculosis, vaccines and immunotherapy. He used to go to TB sanatoria in India, where he saw many HIV patients who developed TB, which he calls “one of the most opportunistic infections among HIV infected people.” He developed an interest in vaccines and joined Emory.
In his immunotherapy study, anti-HIV medicines are combined with an antibody to PD-1—programmed cell death protein 1. PD-1, the discovery of which won the Nobel Prize in 2018, is a protein which regulates the immune system's response. While this prevents autoimmune diseases, it can also prevent the immune system from killing harmful cells and tumours. Therefore, an antibody to PD-1 can make the immune system more 'aggressive' and thereby help reduce the viral load faster—40 days as compared with 150 days for treatment with anti-HIV drugs only. PD-1 antibody is also used in cancer treatment.
According to Amara, only one in 500 sexual exposures results in HIV infection—the process is so inefficient through a mucosal transmission. But the odds of contracting HIV through a needle prick and consequent exposure to infected blood is 100 per cent. A majority of the HIV infections though do occur through sexual intercourse.
Now, HIV is a chronic manageable disorder and has better and cheaper treatments that are being used all over the world, says Dr Ishwar Gilada, president, AIDS Society of India and governing council member, International AIDS Society. “Almost 82 per cent of HIV positive people globally are using anti-retroviral treatment, using medicines made in India at 1 per cent to 5 per cent of the international cost,” he says. “It is very effective HIV treatment that makes the infected person undetectable within three to six months—as a principle, undetectable is untransmittable.”
However, experts say that the prevalence of HIV is still increasing among some populations. “The prevalence is pretty wide from 0.1 per cent to around 20 per cent in some areas,” says Derdeyn. “Some areas have more access to antiretroviral therapies that can impact transmission, some do not. So it is a really heterogeneous mix.”
The pandemic led to a lull in vaccine research. However, learnings from Covid vaccine research have changed the course of HIV vaccine research across the world. The success of mRNA technique in Covid vaccines offers much hope to HIV vaccine researchers. In fact, the Moderna-International AIDS Vaccine Initiative phase-1 study, is now in progress at the George Washington University, Washington, DC.
“The previous shortcomings of HIV vaccine trials are likely to be corrected with the novel approach of mRNA; the results of animal trials using mRNA technique are quite encouraging,’’ says HIV specialist Tejaswi. He is hopeful that HIV vaccines using mRNA techniques will be a reality in the future.
Though no vaccine has yet been licensed by the WHO, efforts have been on for decades. The first candidate vaccine was developed in 1987 and tested in 1989 in a phase-1 trial by Dr Jonas Salk, the inventor of the polio vaccine. Since then, 70 candidates have been developed. “But, only two of them went to phase-3 trial,” says Gilada. “Maybe six or seven went to phase-2.”
The six-year-long RV 144 clinical trial conducted in Thailand, involving more than 16,000 HIV negative volunteers, generated a lot of buzz after its efficacy findings came out in 2009. Volunteers who were vaccinated had a 31 per cent lower rate of HIV infection. Nonetheless, it fell short of expectations as it could protect people from HIV only to a limited extent. Will the DNA/MVA vaccines turn to be another damp squib? “It is too early to comment,” says Dr Prakash Kothari, a sexologist in Mumbai. “But I'm very positive. Anything that increases or improves immunity will be the thing that helps HIV positive patients.”
The vaccines being developed by Emory are based on stronger immune responses and are much better than RV144 vaccine in animal models, says Amara. “My lab has added adjuvants that would actually give us better protection. So we are very hopeful that we will have a better outcome,” he says.
Amara does not fear failure. A firm believer in karma, he is just focused on putting his best foot forward.