Sumaiyya Shaikh was only nine when sweetness as she knew it was cut off from her life. A resident of Malad in Mumbai, she was diagnosed with type 2 diabetes. That diagnosis continues to haunt the 13-year-old even today. “It is frustrating and depressing. I have been asked to eat vegetables all the time. Only a fistful of rice is allowed. I feel so hungry, but cannot munch on anything of my choice because the doctor says everything spikes the sugars. I am a foodie. I love to binge on snacks, noodles, pasta and non-vegetarian food,” Shaikh tells THE WEEK. It is just two days before her birthday, and the usually cheerful and talkative teenager is distraught she cannot even eat cake on her birthday. “It has become such a nightmare,” she rues. Her mother, Nafisa, says she has lost count of the number of medicines Shaikh has consumed to keep her weight in check, because that is where it all began. Shaikh weighs about 60kg.
And, it was her weight that brought her to Dr Akanksha Parikh, paediatric endocrinologist at Kokilaben Dhirubhai Ambani hospital, four years ago. “She had come to me with obesity, and in the process got diagnosed with type 2 diabetes,” says Parikh. “In her case, both her parents are diabetic. If the parents are diabetic, the child will get it 10 to 15 years earlier than the age at which the parents got it. That explains the early onset of diabetes [in Shaikh].”
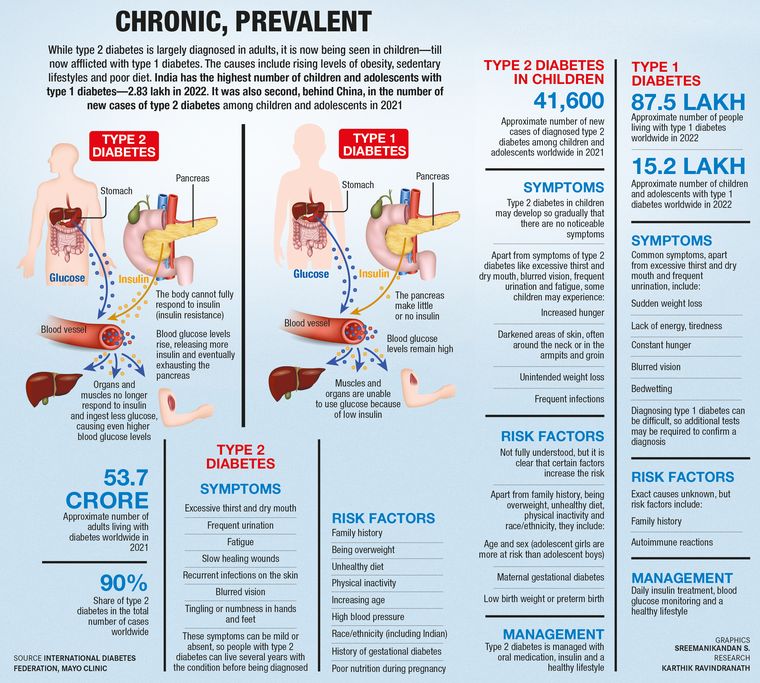
Shaikh was the youngest patient with type 2 diabetes that Parikh had ever seen. Type 2 diabetes is usually seen in adults and not in children. Till recently, children used to be diagnosed with only type 1 diabetes. In type 1 diabetes, the pancreas does not make insulin―the hormone that helps cells absorb glucose from blood―as the immune system attacks the insulin-making islet cells in the pancreas; whereas in type 2 diabetes, the pancreas makes less insulin.
Shaikh was started on insulin therapy initially, and once her glucose control improved she was put on oral medication. “She did achieve good control, but soon her lifestyle went for a toss,” says Parikh. “Children this young are not able to sustain lifestyle discipline for a long period of time. The situation worsened so much that we started her on another anti-diabetic medication (liraglutide) in the form of a daily injection to control the blood sugar.” Liraglutide was recently approved by the Food and Drug Administration for use in children. It helps in increasing insulin levels post meals. Shaikh, says Parikh, was counselled on proper diet, “but her levels of physical activity did not improve despite the counselling”.
Likewise, Harshit Vadher, 17, had to be given insulin injections to control his blood sugar levels. The Virar resident dreams of being a doctor and is preparing for NEET (National Eligibility cum Entrance Test). “The stress of cracking a competitive exam like NEET is so high that his sugars often fluctuate,” says his mother Mayuri. “There is no time for anything except studies and he invariably ends up bingeing on snacks at home.” Vadher’s diagnosis came as a shock to the family as no one in the family is diabetic, adds Mayuri. “His physical activity had dramatically reduced as studies had taken priority,” she says. “But who knew that being studious would invite diabetes? He had sudden weight loss of around 15kg in a short span, which led to the diagnosis.” Until his readings improve, Vadher will have to continue taking the liraglutide injections. He also has diet restrictions. “At times, it breaks my heart to see him burdened with a million restrictions relating to food intake,” says Mayuri. “He is 85kg now. Diet, as prescribed by the dietician, is highly controlled, which means only two chapatis and overall limited carbs. Now, his body has gotten used to the limited meals. For snacking, I give him fox nuts, dry fruits, fruits and salads, but no sugary sweets. He has plenty of self-control when it comes to food, but no time for exercise.”
Doctors across India's major cities agree that there has been a rise in type 2 diabetes among children under 18. “Recent statistics tell us that India houses the second largest number of youth below 20 years with type 2 diabetes,” says Parikh. “The most common age is when they are peripubertal, that is 10 years and above, and from 15 to 19 years because puberty itself is a physiological state of insulin resistance. So, during puberty, they are at a higher risk of glucose intolerance. At the time of diagnosis, HbA1c of some children can be as high as 12 to 16. Anything more than 6.5 is considered to be diabetic range. The fasting blood sugar in these children can go over 200.”
In Vadher’s case, his sugars had suddenly shot up to 600, and he had to be hospitalised. As this was during Covid-19, it was a challenge to find a bed for him. “He looked absolutely normal but the doctor said that his internal organs would be highly affected if he continued with his Covid-induced lifestyle,” says Mayuri.
A lot of these patients are undiagnosed for long because this is an insidious condition, say doctors. Usually, children come to doctors seeking treatment for some other condition, and that is when diabetes is picked up. “Children come to us with complaints of obesity, excessive thirst, frequent urination and sudden weight loss,” says Parikh. And, obesity is a strong risk factor for type 2 diabetes in children. “The increase in body weight is the major reason why children are getting type 2 diabetes,” says Dr Brij Makkar, obesity specialist and president of Research Society for the Study of Diabetes in India. “Almost every week, I see a child with type 2 diabetes. Kids, aged 10 to 12, first enter the pre-diabetes stage and eventually turn into diabetics in a few years. Their HbA1c levels may not be very high but their sugar levels are abnormal, in the range of 126 plus, which is the cut-off for fasting glucose levels, and the postprandial (after food) glucose levels going up to 200 plus.”
Type 2 diabetes progresses more rapidly and aggressively in children than in adults. While adults may be put on oral medication for 15 to 20 years before their pancreas get tired and they are forced to take insulin injections, insulin dependency happens earlier in children as their pancreas work much more than an adult’s for the same amount of glucose control. While there is a gamut of medicines for adults, there are a limited number of FDA-approved medicines for children because of lack of research. Most medicines that are used are purely on an experimental basis. Also, when children have early onset of diabetes, there is a high risk of complications related to kidneys, heart and eyes as they grow up. “What you would have gotten at 60 or 70 years, you will get at 40 years,” says Parikh.
In its recent report in The Lancet, the Indian Council of Medical Research along with the department of health research and the ministry of health and family welfare referred to diabetes as an epidemic and concluded that the prevalence of diabetes in India is considerably higher than previously estimated. “There are serious implications for the nation, warranting urgent state-specific policies and interventions to arrest the rapidly rising epidemic of metabolic non-communicable diseases in India,” the report reads. While this cross-sectional survey primarily assessed a representative sample of individuals aged 20 years and older, drawn from urban and rural areas, doctors across the country are expressing concern about the “potential epidemic” of type 2 diabetes among children as young as eight to ten years.
Doctors began observing this increase in the number of children with type 2 diabetes just before Covid-19. “Four to five years ago, most children who came with diabetes were either type 1 or had pancreatic diabetes (pancreas experiences damage, affecting its ability to produce insulin),” says Dr Shrinath Shetty, consultant endocrinologist, KMC hospital, Mangaluru. “Of late, we are seeing a sudden spurt of type 2 diabetes in children, which was previously uncommon even in those below 40. We started seeing this increase in numbers just before Covid-19. In fact, we assumed it was type 1 initially, but later realised it was type 2. After Covid-19, the incidence has become worse.”

Dr Sreejith Kumar, who runs a diabetes care centre in Thiruvananthapuram, says he is increasingly seeing young patients with acanthosis nigricans, an abnormal darkening of the skin around the nape, the most common tell-tale sign of insulin resistance. “Many parents mistake it for dirt but it is a sign of diabetes in children who are obese,” says Kumar. He cites the example of a 13-year-old girl with the condition. She weighed 80kg and complained of frequent urination, abnormal thirst and fatigue. The girl also had a family history of diabetes. “Children with a family history of diabetes should be extra careful,” says Kumar. “It is very common for young girls with acanthosis nigricans to show abnormal hair growth, polycystic ovarian disease and irregular menses. Managing their lifestyle is the only solution here.”
Sedentary lifestyle, stress, bingeing on junk food and poor protein intake―all of which lead to obesity―are primary factors for the rise in type 2 diabetes in children, say endocrinologists and diabetologists. “Most kids who came to us used to snack a lot on junk food on an almost daily basis,” says Shetty.
One of his patients is a 13-year-old who came to him when he was 11 and weighed over 90kg. He complained of muscle pain, weakness and frequent urination. His parents initially did not take it seriously, brushing it off as viral fever. “He was brought to the casualty in an unconscious state,” recalls Shetty. “It was found that his sugars had shot up to 500-plus. He was shifted to the ICU and started on insulin infusion.” Even after his condition improved, he continued to be on insulin. “During followup, we realised that his body was producing enough insulin but just that because of bad food intake and a sedentary lifestyle, he had become diabetic, which went unnoticed for a long time,” says Shetty. “He also had weakness in the leg that improved with physiotherapy and cycling. After months of insulin dependence, he was shifted to medication― metformin 500mg―which has been reduced to half a tablet every alternate day. Being a single child, he was pampered. His tantrums were always given in to and he would end up ordering junk food every day. With a shift in dietary habits, he is now at 70kg.”

But is it fair to expect children to lead a disciplined lifestyle with diet control, ask parents. The inability to control cravings, frequent hunger pangs, peer pressure and tempting food make it next to impossible for children to stick to a diet, they say. This results in frustration, irritability and frequent arguments between parents and children. “It all started during the lockdown,” says Swapnali, mother of Mayank, 10, who is an avid footballer and cat lover. “That was the time when my boy also gained weight because there was nothing else to do except sit at home, stay glued to the phone screen and munch.”
Swapnali, a single parent, never thought of checking Mayank’s sugar levels, despite her mother being a diabetic, as he had a normal weight earlier and was active in sports. “A persisting high fever led to the diagnosis and our tryst with diabetes began,” she says. And in came diet and discipline. “Despite trying so hard, at times it is natural to slip, especially when a young child is involved,” says Swapnali. “When his friends have a party downstairs, he enjoys treats without even telling me. At home, in my absence, it is difficult for him to stick to a schedule, and an erratic schedule disrupts the sugar levels. So this is a catch-22 situation we find ourselves in. Though I am lucky that my little boy shows loads of self control, there are times when he gives in to temptation.”
The problem, says Shetty, is that once a patient becomes better, they do not follow up or take it lightly and this is very dangerous as far as diabetes is concerned, especially among children because the counts fluctuate all the time. “What happens in children is sometimes because of the school schedule, their health takes a backseat,” he says. “That is why, we must see children once in three months for sure.”

The youngest type 2 diabetic patient that Dr Lenatha Reddy from Rainbow Children's Hospital, Hyderabad saw was also a ten-year-old. “He was obese and his HbA1c was 7,” she recalls. “With medication, his parents are trying to bring the markers within a normal range.” The boy had come to her before Covid-19. “Post Covid, this has become more alarming, with children getting addicted to mobile phones and staying indoors for two to three years and eating highly processed foods,” she says.
There is also a theory that birth weight has a direct link to being at risk for diabetes later in life, says Reddy. “Babies who are underweight and those who are overweight at birth are at risk of having diabetes when they grow up,” she says. In babies who weigh less than 2.5kg at birth, the weight gain is usually brought about rapidly, which puts them at risk of metabolic complications later on. “The problem is that in our society we tend to normalise obesity in children as healthy,” says Reddy. “But it is only when your BMI is okay for your age and sex that you are actually healthy as a child. Do not feed children excessive calories with the idea of a rapid weight gain because that translates into visceral fat. This is responsible for the onset of diabetes, and Asians are at a higher risk because of our thin-fat phenotype (increased body fat in an individual with normal BMI) as against Caucasians.”Recently, Dr Arun Menon, an endocrinologist at Amrita Institute of Medical Sciences, Kochi, attended to a 20-year-old nursing student with a normal weight who “did not show any alarming symptoms”. She had lost a bit of weight but attributed it to living in a hostel. Her cholesterol was normal and so were other parameters except sugar levels―they were abnormally high. Menon initially thought she had type 1 diabetes, but she turned out to be a lean type 2 diabetic―people who are not obese but have severe insulin resistance. “We can only speculate about endocrine disruptors, food adulteration or other lifestyle-related factors, but the real reason is difficult to pinpoint,” he says.
There is one thing Menon is sure of. “We are all at risk, given the way this epidemic is spreading,” he says. “We are now getting cases on a weekly basis, as against monthly. The spread has increased four to five times in five years.” Another shocking aspect that he observed among children with type 2 diabetes is that very few of them have a family history of the disease. “For those who do, their parents must have gotten this disease in their 50s,” he says. “However, by the next generation, this will [happen] 20 years earlier. I have noticed that at least 40 per cent of patients who come to the hospital for any disease have diabetes. Because this is the very first time we are seeing children this young with diabetes, it remains to be seen how they grow up and grow old. It is scary that these children may go on to face major medical problems by the time they hit their 30s because this is a chronic disease and it might take 15 to 20 years for the disease to manifest. This is only the start of their journey. And it is a huge population, not just a few people.”
Dr Jugal Kishore, who leads the community medicine department at Delhi's Safdarjung hospital, has been visiting schools in New Delhi to look for adolescents with diabetes. “Most of these kids are obese, so much so that their BMIs range between 30 and 40,” says Kishore, who is general secretary of the Indian Association of Adolescent Health. “We find out diabetes only when they undergo checkups for other problems such as pneumonia.”
He cites the example of a school in Bengaluru. “There the prevalence of obesity among children has been increasing rapidly in the last ten years, from 10 per cent to 15 per cent,” he says. “In Delhi, the same is 20 per cent and above. In private schools catering to the upper middle class, it is 25 per cent.”
Children also face stigma in schools. “My teacher asked me not to attend the school picnic because I am diabetic,” says Shaikh, rolling her eyes. “What if something goes wrong with me when I am outdoors?”
Experts say that children should have moderate to vigorous physical activity every day for 45 minutes, “which means they should sweat and their heart rate should go up and they should be breathless while performing the activity,” says Shetty. “When these three things happen together for five days, we say that there is adequate physical activity.”