As the car rolled up a winding path lined with trees, I wondered if we were indeed visiting a research centre. A tall building with a curtain wall façade—that is the picture most of us have of a scientific research centre. This centre was anything but that, with massive pillars at the entrance, intricate etchings, statues of majestic lions, floors with elaborate patterns and slanting roofs with grooved terracotta tiles. “Welcome to the Satelmond Palace!” said a staffer. Confused yet overwhelmed by the beauty of the place, I walked in and saw a whole different world hidden in what was once a royal residence. Who thought a palace could be converted into an extensive biomedical research centre! You will find everything, from testing labs, research and development cells to conference halls and an animal house, at the Biomedical Technology (BMT) wing of the Sree Chitra Tirunal Institute of Medical Sciences and Technology (SCTIMST)—all set up without destroying the traditional architecture of the palace.
The BMT wing, about 11km from SCTIMST and away from the hustle and bustle of Thiruvananthapuram, was designated as a technical research centre for biomedical devices by the Union government in 2016. And, it has played a leading role in establishing a medical device base in India by successfully developing and transferring technologies of diverse medical products.
The centre’s royal connect dates back to Maharani Sethu Lakshmi Bayi, granddaughter of the celebrated painter Raja Ravi Varma. She lived in the Satelmond Palace in Poojapura and ruled erstwhile Travancore as a regent on behalf of her nephew Maharaja Chithira Thirunal Balarama Varma. The Malayala Manorama described her reign as the golden age of Travancore. The queen’s portrait still hangs in the hallway at the entrance of the main building.
Past the hallway is the library, with old shelves in shades of mahogany lined in rows, half-open reading cubicles and fat, hardbound books with ivory-hued pages. Every cubicle had a person reading a book or taking down notes.
A set of wooden stairs took us to a conference room and a grand dining area. As I headed to the next set of stairs, which probably led to the attic, a staffer said, “It is better not to go up; some of the stairs are shaky and some broken.” My curiosity subdued, I headed in the opposite direction. But this made me question the stationing of the research centre at a palace so rich in history—should it not be a museum instead? “What is better—preserving history or creating it?” asked Dr P.R. Harikrishna Varma, head, BMT wing. “We are doing both.”
After the Maharani moved to Bengaluru to be with her daughter and grandchildren post independence, the palace stood neglected. In 1972, chief minister C. Achutha Menon invited Dr M.S. Valiathan, a cardiothoracic surgeon, to set up a mutlispeciality hospital in a building gifted to the Kerala government by Chithira Thirunal. Valiathan also wanted to promote medical research; he asked the queen for the use of the palace. She agreed, and the BMT wing came up there. “The BMT wing is not just a significant part of history, but it is also in the process of scripting stories that will one day go down in history,” said Harikrishna.
As we enter the 3D printing lab, we are asked to change into lab slippers. “It is part of good lab practices,” said a research scientist. With sanitiser bottles at every corner, staffers are expected to prevent any possible cross-contamination. “The key focus area of the 3D printing lab is development of tissues, organs and other biomaterials for testing of medicines. Even artificial skin is developed here; this would be very beneficial to the cosmetic industry as they can perform testing of their products on 3D printed tissue,” said Harikrishna. Even the entry doors of the microbiology labs swing inwards to prevent outflow of contaminated air.
“We have a well-trained and committed team of engineers, scientists, clinicians, public health experts and technicians as well as unique research, development as well as testing facilities—all under a single roof, working towards radical innovations to improve health care facilities,” said Harikrishna. A behemoth in the research field, the institute holds several national and international patents for devices and processes developed under various programmes. Some of the technologies are in production. With a series of new products and technologies under development, their vision for 2030 focuses on nine areas—cardiovascular devices, neural prostheses, orthotics and rehabilitation, in vitro diagnostics, hard tissue devices, biologics, regenerative technology, point-of-care devices and connected health. Here are the top five technologies by the BMT wing that are at different stages of development.
VEIN VIEWER
Ever got into a tiff with a nurse for getting jabbed in the wrong place? Most people dread blood tests for this very reason. This can be nerve-wracking for the nurse, too. Spotting veins just got easy, thanks to the vein viewer device that uses near-infrared light to visualise the veins. “This is a great tool to prevent needle-stick injuries and make blood tests and intravenous drips less miserable. It comes in both hand-held and hands-free models,” said Sarath S. Nair, scientist. Though there are other vein finders in the Indian market, the BMT’s vein viewer displays a larger area of the skin.
BIOCERAMIC BEADS
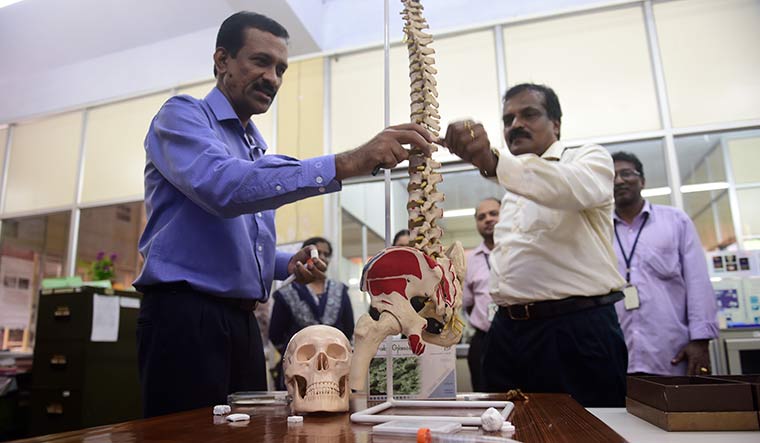
We then moved to material science, Harikrishna’s area of interest. Enter a large lab with models of bones, and a bunch of enthusiastic scientists gather around to talk about bioceramic beads. “Bone infection or osteomyelitis is one of the most dreaded complications after trauma and implantation,” said Harikrishna. As there is low blood flow in the bones, systemic antibiotic treatment is less effective. The best way to treat it is on-site delivery of antibiotics. “Currently, bead-shaped PMMA (polymethyl methacrylate) bone cement loaded with antibiotics is used. The implanted beads are to be surgically removed later as they cannot be resorbed,” he said. According to him, the new bioceramic beads, designed with micro-nano porous structure, deliver the antibiotic and later get integrated with the host bone. Therefore, there is no need to surgically remove the beads later. These beads are also used to fix spinal injuries.
ORALSCAN
We got out of the material science building and climbed another set of stairs till we reached a quiet corridor, with just a row of cabins. No lab equipment or researchers in white coats here. “This is our business incubation centre—TIMed. We have about 10 startups now,” said Harikrishna . We stopped at one of the startups—Sascan Meditech Private Limited. “We develop a scanning device here,” said a staffer. And not just any scanning device, this one identifies cancer sites in the mouth. With increased use of tobacco and alcohol, oral cancer is no longer a rare ailment. Thanks to OralScan, diagnosing the disease is as easy as taking a photograph. The common sites of the cancer are tongue, lining of the lips, floor of the mouth and upper throat and then it spreads to other regions. Most people ignore the symptoms as it usually starts as a painless white patch, which then thickens and turns into red patches and continues to grow. Or, it can be a persistent ulcer on the lips that does not heal. “Early screening and detection of oral cancer is usually difficult owing to the lack of affordable screening techniques, painful procedure and high costs,” said Subhash Narayanan, founder and CEO, Sascan Meditech. “OralScan solves this issue. It has a noninvasive intraoral multispectral imaging camera. It detects cancer from tissue fluorescence and diffuse reflectance and identifies the most malignant site for biopsy. It is so user-friendly that health workers with minimal training can also operate it.” The two-piece device includes a hand-held scanner and a tablet that generates images of the scan.
TB TESTING DEVICE
According to the World Health Organization, India accounts for the highest number of deaths due to tuberculosis. “Currently, there is no device to screen a mass of people,” said Dr Anoop Thekkuveettil, scientist, division of molecular medicine. “If we do the screening in India, I think all of us will show TB positive because at some point in our life, we have been exposed to the infection.”
TB is highly treatable, but most people ignore its early symptoms. Also, multi-drug resistant TB cases are on the rise, hence the faster it is screened, the sooner it can be eliminated. According to Anoop, the WHO has mentioned that skin-based test can no longer be performed in India for the detection of the disease; it has to be DNA-based. “Currently, there is a machine that can test four samples at a time and takes around three hours to complete the process,” he said. “In this case, around 12-14 samples are tested a day. In Kerala itself, we have around 20-25 patients who are suspected to have [MDR-TB]. So, there has to be a system that will enable faster detection.”
The device developed by his team can test 20 samples simultaneously within 20 minutes, said Anoop. “SCTIMST has patented the device and it is going to be game-changer for our country,” he said. “The device costs only Rs10,000 and it has high specificity. India has a vision to completely eliminate the disease by 2025, but we are nowhere close to even detecting the infection. If this device is supplied to all the peripheral centres across the country, then we can diagnose and treat the disease in its early stages.”
UTI DETECTION KIT
A urinary tract infection (UTI) is usually self-diagnosed based on several minor symptoms like a persistent urge to urinate, burning sensation while urinating, cloudy, red or cola-coloured urine and pelvic pain. It is an infection in any part of your urinary system—kidneys, ureter, bladder and urethra. It is not always serious but if not treated, it can affect the functioning of the kidneys. At the BMT wing, Dr Maya Nandkumar, scientist and head, department of microbial technology, has developed a self-contained detection kit with her team. “Collect 3ml of the urine sample and add to the vial in the kit with injection water,” she said. “With the help of a dropper, transfer 0.5ml of the sample to 12 different vials with different antibiotics and leave it for two hours. The colour of the liquid will be green initially, it will turn to orangish yellow if the sample has the infection.” The kit also helps identify the antibiotic that will aid treatment; the vial with no change in colour is the one with the antibiotic that will work. “It can be easily performed in an outpatient clinic or primary health centre without a lot of training,” said Maya.
According to her, every technology has its own uniqueness. “As scientists, our responsibility is to identify a need and then invent a technology that caters to it,” she said. “The happiness we get through this is beyond words.”