The path lab holds secrets, both good and bad. As nurses go in and out of the dimly lit room, curious eyes try to scan the files they hold. “John,” the receptionist calls out. A healthy young man approaches the desk. His file reads, ‘biopsy report’. John takes a deep breath and flips the pages. Before he could finish, a nurse gently takes it from him and takes him to a doctor. As he follows her, the 28-year-old Googles for the medical jargons he remembered seeing. He need not have.
The confirmation comes like a whiplash, tearing into his young life. Testicular cancer, it is, and John’s hands tremble. Questions swirl around inside him. “Is it fatal? How did this happen? I am a teetotaller and still? Will I be able to get married and have children?” His head swimming, John walks out of the room with a slip for his next session.
Age is not a factor when it comes to cancer―it can happen to anyone at any time. Despite the fact that most young people delay starting a family or don’t fancy the idea of rearing children, infertility is something that scares people in this group.
Says Dr Arun Warrier, oncologist, Aster Medicity, Kochi: “Testicular cancer is rare and is most common in males between the ages of 15 to 34. But there is no reason to fret, as it can be highly treatable even when it has spread beyond the testicles. Though, it is possible that the fertility gets restored after four to five years, doctors usually ask the patients to go for cryopreservation of sperms, especially if they have not started a family.”
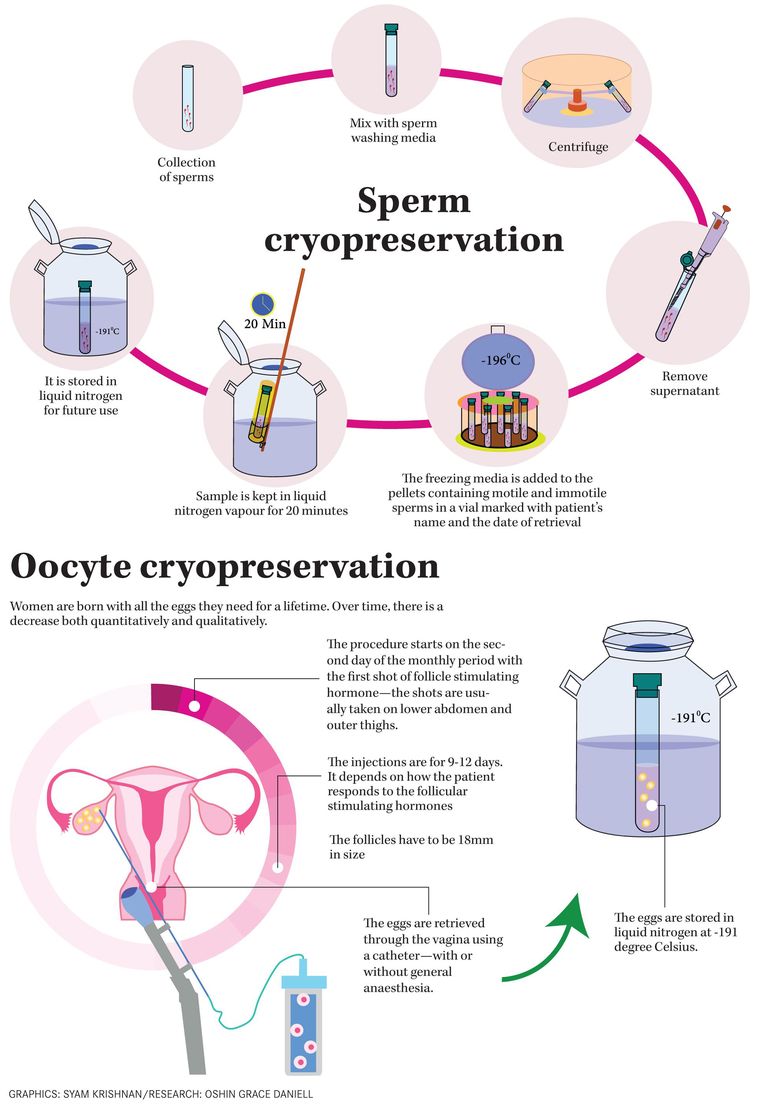
Cryopreservation involves preserving biological materials at extremely low temperatures (mostly -191 degree Celsius) in liquid nitrogen. It prevents all biochemical reactions that lead to cell death―which is key when it comes to preserving germ cells for future reproduction.
Most people think that only genital cancers tend to affect fertility. But that is not true. Chemotherapy or radiation therapy for any type of cancer can affect fertility. Besides that, bone marrow transplantation in patients with lymphoma—cancer that begins in the cells of the immune system—can cause infertility. It can result in menopause among women. “The cancer cells as such don’t have an effect on fertility but the medicines and treatment to kill these cells do. Post chemo or radiation therapy, it takes about three to five years for the body to get back to normal. We tell our patients to wait for at least three years before they think about starting a family as the quality of the sperms will be poor in this period,” says Arun.
The situation is a little more complex when it comes to women. According to Dr Shameema Anvar, gynaecologist, Aster Medicity, Kochi, “Chemotherapy or radiotherapy can affect the reserve of the ovary, which in turn reduces fertility. Unlike semen which can be collected on any day and contains millions of sperms, the ovary produces a single egg in every cycle―28 days. When we go for cryopreservation of oocytes, medicines are administered for stimulating the ovaries to produce multiple eggs. This can take around 10 to 14 days.”
In case of ovarian cancer, the affected ovary is removed and the other is functional. Although, there is a reduced quantity of egg, natural conception is possible. But, it is not as harmful as breast cancer. “Nowadays, we see a lot of young women, between ages of 25-40, with breast cancer.
Chemotherapy cannot be avoided in this case and the drugs used in therapy can impair fertility. In order to shield the ovary, we administer ovarian suppression drugs which temporarily ‘shuts down’ the ovary. Chemo-induced amenorrhea is common in breast cancer cases―an early menopause kills the chances of naturally conceiving a child,” says Arun.
The big question is, are people sensitised about this? Says Dr Mathew Pappachen, fertility specialist and clinical embryologist, Lifeline hospital, in Kerala: “Proper counselling is key when it comes to dealing with cancer and cryopreservation prior to its treatment. The journey can be less traumatic if patients are made aware of all the complications and factors that they need to keep a tab on, both before and post treatment. Though the causes of infertility are attributed to physiological factors, the stress and heartache associated with it―often exacerbated by treatments―can have a huge psycological impact.”
Most people tend to focus on the disease and not its impact. “Patients usually want us to eliminate the disease; they don’t think of any precaution to fight the impact of the ailment. They hurry into the treatment and some don’t heed to our advice to preserve their egg or sperm,” says Arun.
Collection and storage
The simplest method of producing a semen sample for sperm banking is masturbation. But, there are other techniques available if this is not possible. In cases associated with disruption of the ejaculatory reflex arc such as in spinal cord injuries, electroejaculation is apt―this requires a general anaesthetic though. Another technique is surgical sperm retrieval― epididymal sperm aspiration and testicular sperm extraction are performed when there is a low sperm yield. In certain cases, epididymal sperm can be retrieved by percutaneous epididymal aspiration (PESA). If PESA fails then testicular sperms are obtained by needle aspiration biopsy (NAB). After collection, the sperm is prepared for freezing at -191 degree Celsius.
Semen collection is simple when compared to collecting oocytes. The procedure takes around two weeks. “Patients are administered medicines to produce hormones that stimulate the ovary to produce eggs. These eggs are sometimes collected under general anesthesia. These eggs can be cryopreserved or fertilised in vitro to embryos in case the woman is married. Embryo cryopreservation is more effective than freezing oocytes,” says Shameema.
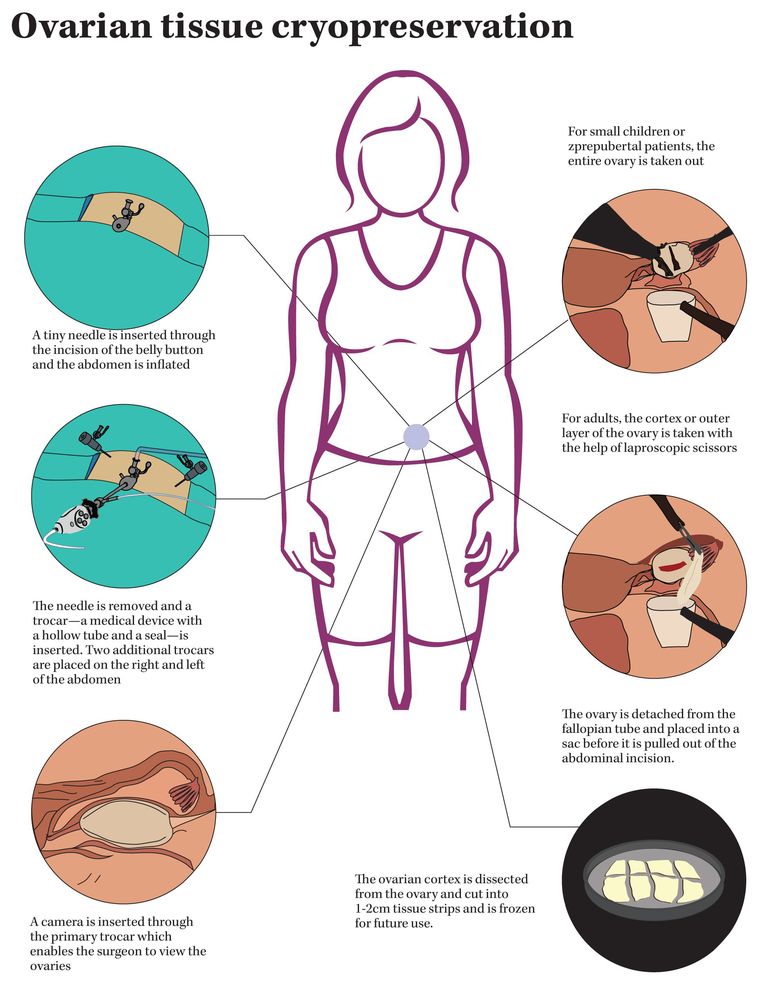
When it comes to prepubertal, ovarian tissue freezing is the only option. Both chemotherapy and radiotherapy cause loss of ovarian function due to follicular depletion. According to Dr Mathew, both oocyte and ovarian tissue cryopreservation is 100 per cent effective when it is done right. “Ovarian tissue cryopreservation, though an experimental method of fertility preservation, has the advantage of not requiring an ovarian stimulation. This is ideal for patients who cannot delay their cancer treatments as oocyte cryopreservation takes around two weeks. Unlike freezing individual oocytes or embryos, ovarian cryopreservation can preserve hundreds of primordial follicles at once,” says Mathew.
Social freezing
Apart from cases in which the person has an ailment, social freezing is becoming very popular. “Many young people who are very focused on their career mostly go for delayed marriage and hence, they postpone parenthood. As the quality and quantity of egg and sperm decreases with age, it is advisable that cryopreservation is performed in their early reproductive years,” says Shameema.
Although this trend is popular among celebrities, many young people now opt for this method as a precaution. Despite the fact that a lot of controversies revolve around the ethical aspect this concept, the numbers tell a different story.
Patients with disabilities, especially spinal or in the lower abdominal region, also opt for cryopreservation as the disability can affect physical abilities to engage in regular sex. “We have had patients in their early 20s who got paralysed hip down after accidents. In such cases, we ask the patients to go for cryopreservation so as to avoid complications in the future. It is also possible to retrieve sperms from the epididymis of male, within a few hours after death,” says Mathew.
Be it social or medical freezing, the technique is a ray of hope for many across the world. The future looks at extracorporeal gestation―pregnancy outside the body using an artificial uterus―to free women from the constraints of biology and time. Surely, social freezing would play a significant role in the aforementioned. Since egg freezing lengthens the time during which a woman can get pregnant, it levels the field when it comes to biological differences between men and women. Apart from its physiological benefits, egg freezing promotes equal participation in employment and educational endeavours; it also gives more time to become psychologically and emotionally ready to be a parent. Maybe, the delay is empowering―or maybe not. To wait or not to, is the question.